Blood Counts for Patients Receiving Chemotherapy or Radiation Therapy

A complete blood count (CBC) is a blood test done to help your child’s doctor or health care provider know more about their condition. It shows how many white blood cells, red blood cells, and platelets are in their blood. If your child is getting chemotherapy or radiation therapy, their blood needs to be checked often to see how the treatment is affecting their blood cells. Your primary cancer and/or radiation doctor will tell you how often labs need to be checked.
A CBC is done by taking a sample of blood from your child. This is done by a needle and taken from a vein, a finger stick, or a central line if you child has one and it can be used.
Blood
Blood carries oxygen and nutrients to all parts of the body.

Bone Marrow
White blood cells, red blood cells, and platelets are made in the soft, spongey tissue inside your bones, called bone marrow (Picture 1). When receiving chemo or radiation, your team will closely monitor white blood cells, hemoglobin, and platelets. Chemotherapy and radiation therapy may damage the bone marrow and the cells in it.
- In babies under the age of 1, blood cells are made in the bone marrow of all bones.
- In anyone over the age of 1, blood cells are only made in the bone marrow of the pelvic bones, breastbone, ribs, and backbone.
White blood cells (leukocytes):
Are needed to fight infection.
- May grow in number when needed to fight an infection.
- Have a normal count in children between 4,000 and 10,000.
- May decrease when receiving chemotherapy or radiation therapy and can become much lower than normal, especially 7 to 10 days after most chemotherapy treatments.
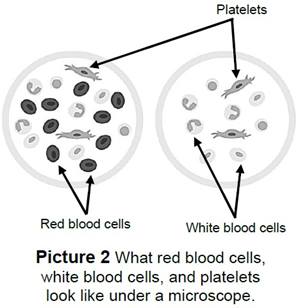
Red blood cells (Picture 2):
- Hemoglobin (hee-moh-glow-bin) carries the oxygen we breathe to all parts of the body.
- Normal hemoglobin level in a child is 12 to 14.
- May decrease when getting chemotherapy or radiation therapy and can become much lower than normal, especially 7 to 10 days after most chemotherapy treatments.
Platelets:
- Help your blood clot to stop bleeding.
- Have a normal count of 140,000 in children.
- May decrease when receiving chemotherapy or radiation therapy and can become much lower than normal, especially 7 to 10 days after most chemotherapy treatments.
Signs and Symptoms
Low Blood Counts
There are different signs and symptoms to look for when your child is getting chemotherapy or radiation therapy. Call the Hematology Clinic if your child has any of these signs:
| Infection |
|
|
||
|
Low blood count |
|
|
||
|
Low platelet count |
|
|
||
Treatment
Treatment depends on what signs and symptoms your child is having.
| Infection |
|
|||
|
Low hemoglobin |
Red blood cell (RBC) transfusion given in an IV over 2 to 4 hours. This is done to increase the RBC count until the bone marrow makes new cells. |
|||
|
Low platelet count |
Platelet transfusion given in an IV for about 1 hour. This is done if the platelet count is very low or if there's bleeding that won't stop. Platelet transfusions lower the risk of bleeding until the bone marrow can start making new platelets. | |||
Prevention
Below are things you can do to help keep your child healthy and safe while they’re getting chemotherapy or radiation therapy.
- Make sure your child and everyone in the family washes their hands well. Always wash hands with soap and warm water after using the bathroom, before eating, and after touching any animals.
- Avoid being around people who are sick.
- Don’t let your child dig in dirt or sand.
- Check with your cancer care team about how your child can help care for pets and what activities to avoid.
- Your child should not clean liter boxes, work in barns, handle or care for birds, mow the grass, ride a tractor, or plow. Keep them away from dusty areas.
- Keep your child from swimming in creeks, rivers, lakes, or oceans. Don’t let them near standing (stagnant) water.
- Be aware of food safety for raw or undercooked food and drinks.
- There may be times during treatment that your cancer team recommends avoiding things like school, high risk contact sports, crowded areas, and other activities that may put you at risk for infection.
When to Call the Doctor
Call your child’s doctor or health care provider if:
- You think they have an infection.
- They’ve been around anyone with the chickenpox or shingles virus.
- They get a cut or scrape that bleeds a lot. Put pressure on the area and use a dry gauze pad for 15 minutes.
When to Call 911
Call 911 for emergency help if your child:
- Can’t breathe.
- Is seriously injured.
- Has a lot of bleeding that won’t stop.
HH-III-76 • ©1990, revised 2023 • Nationwide Children's Hospital
