Poisonings and Poison Prevention
Central Ohio Poison Control
Looking for services or physicians who can help treat this condition?

Children under the age of 5 learn by exploring the things around them. They crawl, walk, put things in their mouth, and grab most things they see. This puts them at a higher risk of poisoning. Things like medicines, chemicals, and gases can be dangerous. They can lead to poisoning if they are swallowed, breathed in, touched, spilled on the skin, or injected.
| If you think your child has come into contact with a poison: | |
If your child has passed out or is not breathing, call 911 or take them to the closest emergency room right away. |
When you call, have this information ready:
- Your child's weight and age
- Any symptoms they're having
- Any medicines they're taking
- Any medical problems they have
- The name of the poison and time they came into contact with it (if known).
- If it was a medicine, have the container or bottle with you when you call.
- If it was a plant or animal, describe it the best you can.
Types of Poisons
Keep these items out of the reach of children and pets:
Medicines and vitamins
- Prescriptions, vitamins, laxatives, and antacids
- Over-the-counter (OTC) medicines, especially pain medicines like aspirin, ibuprofen (Motrin®, Advil®), and acetaminophen (Tylenol®)
Drug-related items
- Smoking products like lighters, cigarettes, vape pens, vaping liquid, weed
- Alcohol drinks like beer, wine, liquor, whiskey, and more
- Edibles - food, usually candy or dessert, that has heated up (cooked) marijuana in it
Cleaning items
- Bleach
- Drain cleaner
- Ammonia
- Oven cleaner
- Pool cleaner
- Toilet bowl cleaner
- Disinfectant sprays or wipes like Lysol®, Clorox®, Microban®
- Laundry detergent (powder, liquid, or pods)
- Dish soap and detergent (powder, liquid, or pods)
- Air fresheners, candles, and wax for wax warmers
Bathroom items
- Mouth wash
- Makeup
- Hair products
- Body oil and lotion
- Rubbing alcohol
- Hand sanitizer
- Nail polish and remover
- Perfume and cologne
Bedroom items
- Purses
- Backpacks
- Button batteries
- Remotes
- Magnets and magnet toys
- Diaper bags
- Anything that uses small batteries
Garage items
- Bug spray
- Fertilizer
- Kerosene
- Wiper fluid
- Weed killer
- Gasoline
- Paint
- Lead paint
- Pool chemicals
- Antifreeze
- Paint thinners
- Tiki torch fluid
Plants
- Fox glove
- Poison ivy
- Poison oak
- Poison sumac
- Dieffenbachia
- Philodendron
Gases
- Propane
- Carbon monoxide
- Methane, natural gas
Signs and Symptoms
Signs and symptoms for poisonings depend on how the poison got into or on the body. There are also different signs and symptoms for different types of poisons. Some common signs are:
- Problems breathing
- Seeming sleepy (drowsy)
- Throwing up (vomiting)
- Acting confused
- Skin redness, irritation, burning, or itching
- Having breath that smells like chemicals, like gasoline or paint thinner
Preventing Poisonings
Be Poison Smart!®
- Watch out for poisons that look like things your child may want to eat or drink. Every time you bring something home, ask yourself:
- Is it medicine or vitamins?
- Does it have alcohol in it?
- Does it have gasoline, insecticides, or pesticides in it?
Medicines
- Never call medicine candy.
- Keep all medicine locked up and out of the reach of children and pets.
- Do not take medicine in front of your child.
- Do not keep pills in a bathroom.
- Do not keep medicine or medicine packaging on counters or window sills.
- Put refrigerated medicines in the very back of the fridge.
- Always read the label before giving medicine. Make sure it's the right medicine and dose for your child.
- Many OTC medicines are not safe it taken incorrectly.
- Never give your child medicine in the dark.
- Keep track of all the medicine(s) your child is taking.
- Get rid of medicines that are not being used or have expired.
- Do not keep medicine in the pockets of clothing.
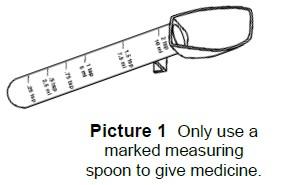
- Do not use kitchen spoons to measure medicine. Use the cup that came with the medicine or buy a medicine measuring tool from any pharmacy (Picture 1).
Locks, lock boxes, and safes
- Keep dangerous items locked up high where your child can't reach them.
- You can also put items away in a lock box or safe (Picture 2). Make sure these boxes are also up high and out of reach.
Containers
- Only use products with child-safe caps. Remember, having a child-safe cap doesn’t mean your child can’t get into it. If they try hard enough, they may still open it.

- Containers for laundry and dishwasher pods must be stored up high and locked up. These are very dangerous and look like something a child may want to eat (Picture 3).
- Keep products in their original, labeled containers.
- Read the product’s name, label, and how much to use before each use.
Plants and outdoors
- Know the berries, fruits, seeds, flowers, shrubs, mushrooms, and trees in your home or yard. If you don’t know the name, take a branch or leaf to your local plant store.
- Teach your child to not touch or eat things they find outside.
- If you treat your yard with pesticides, do not let your child play in outside for 24 hours.
- Keep grills and generators away from windows.
- Clean chimneys and get them inspected.
Carbon monoxide
- This is a deadly gas that you can’t see or smell.
- It can come from a gas stove, dryer, furnace, fireplace, grill, or car.
- Put a working carbon monoxide detector on every floor of your home.
HH-IV-30 • ©1981, revised 2023 • Nationwide Children's Hospital
