The Fetal Center
Caring for Mom and Baby Before and After Birth
Meet Oluyinka Olutoye, MD, PhD
Operating Inside the Womb
The Fetal Center
We know this can be a very stressful time for you. Our expert team of fetal medicine specialists is here to guide and support you each step of the way. Our goal is to provide you with the information and care you need to prepare for the birth of your baby.
As a member of the Ohio Fetal Medicine Collaborative (OFMC), Nationwide Children's offers families facing potentially complex birth defects the highest quality care. The most advanced diagnosis and treatment is available to both the mother and fetus before, during and after the infant’s birth.
Nationwide Children's Fetal Center is a member of the North American Fetal Therapy Network (NAFTNet), a voluntary association of 36 medical centers in both the United States, Canada and Mexico that perform advanced in-utero fetal therapeutic procedures.

Member of the North American Fetal Therapy Network (NAFTNet)
Overview
During your fetal center visit, the pediatric specialists will discuss the diagnosis, treatment, recovery and long-term prognosis of your baby. We are also here to provide supportive care, listen to your questions and discuss your concerns.
Nationwide Children’s works closely with families and their perinatologists to utilize state-of-the-art diagnostic and treatment protocols from a full range of specialties to improve neonatal outcomes for most fetal complications. These specialties include maternal-fetal medicine, genetics, radiology, transfusion services, laser treatment, labor and delivery, neonatology, cardiology, anesthesia, pediatric surgery, urology and neurosurgery.
Conditions We Treat
Learning you have a high-risk pregnancy or fetal abnormality can be very stressful and overwhelming. That’s why we work hard to provide a seamless and collaborative care plan for both you and your baby.
Our expert team evaluates and treats nearly every fetal complication, from the most common birth defects to complex fetal anomalies. By using advanced diagnostic methods, we work to pinpoint the fetus’s condition and recommend the best possible treatment.
We frequently evaluate and treat conditions such as:
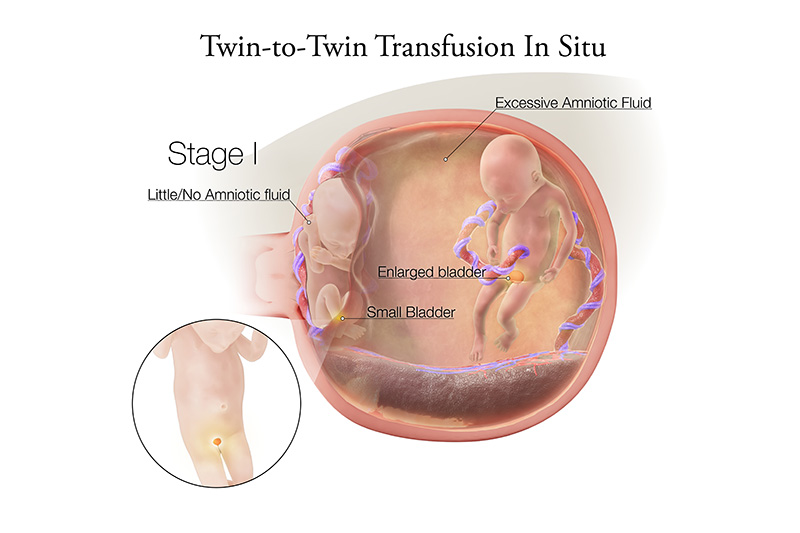
Twin to Twin Transfusion Syndrome (TTTS)
Identical twins who share one placenta may be at risk for Twin-to-Twin Transfusion Syndrome (TTTS). The single placenta contains blood vessels going from one baby to the other. In TTTS, blood from the smaller donor twin is transferred to the larger recipient twin, causing an uneven exchange of blood.
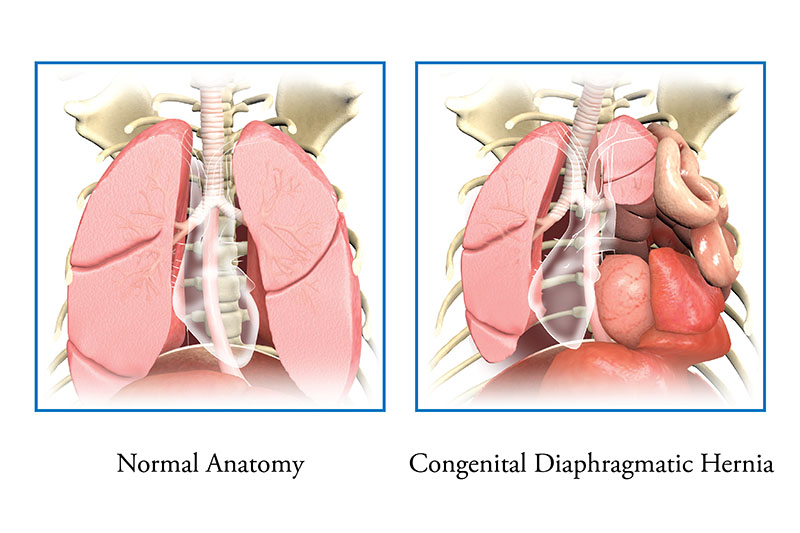
Congenital Diaphragmatic Hernia
Congenital diaphragmatic hernia (CDH), is a rare congenital condition where the muscles in the diaphragm do not grow together, leaving a hole. The hole allows the intestines and other organs (stomach, liver) to move up into the baby’s chest. When this happens, it makes it hard for the lungs to grow.
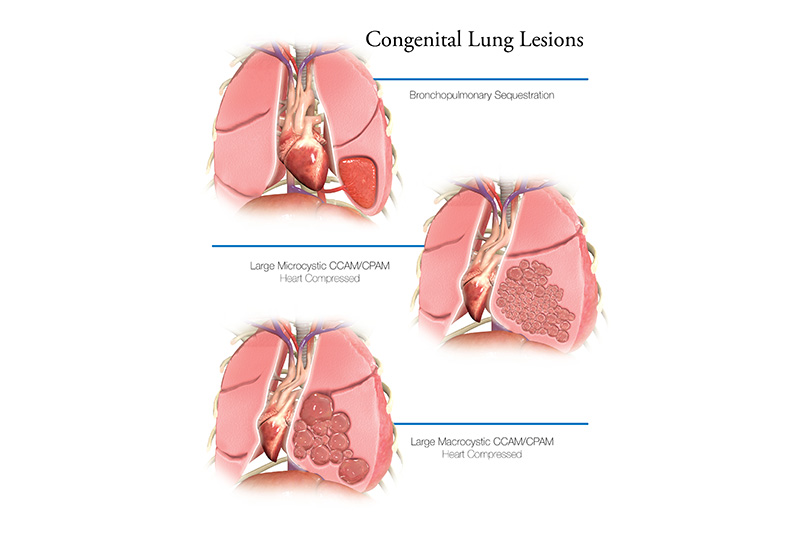
Congenital Lung Lesions
Congenital lung lesions are a group of conditions where part of the lung has an abnormal growth or mass. Congenital pulmonary airway malformation (CPAM), bronchopulmonary sequestration and congenital lobar emphysema are the most common types of congenital lung lesions.
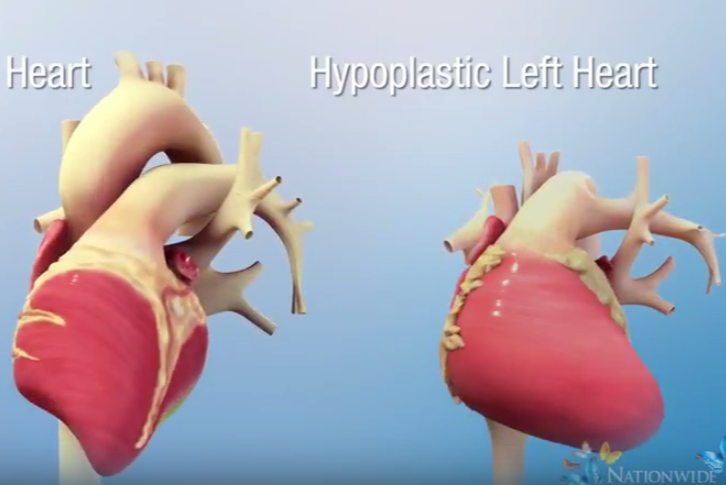
Fetal Congenital Heart Defects
A congenital heart defect or congenital heart disease means your baby’s heart or their heart’s blood vessels are not growing the typical way before birth. Special fetal cardiac care can find and sometimes treat heart defects before your baby is born.
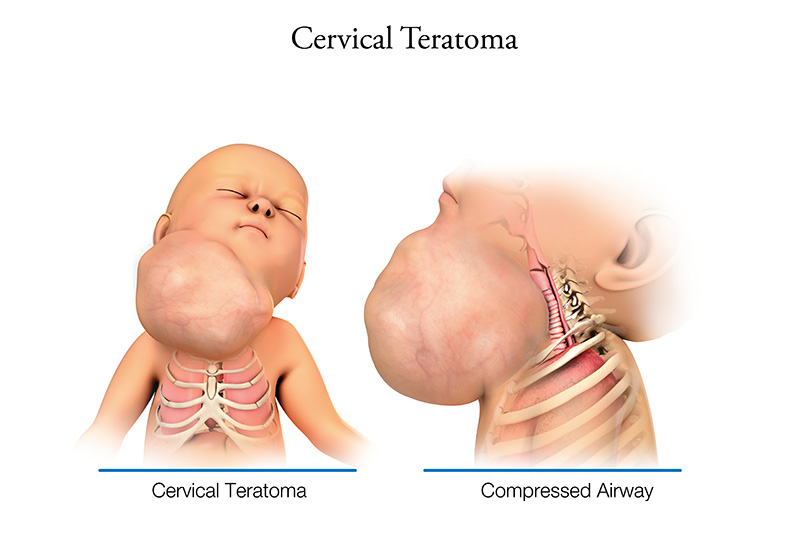
Cervical Teratomas (Giant Neck Mass)
A giant neck mass is an abnormal growth of the neck. There are two different types of masses including cervical teratomas and lymphatic malformations. The cause of it is unknown, but it can be treated.
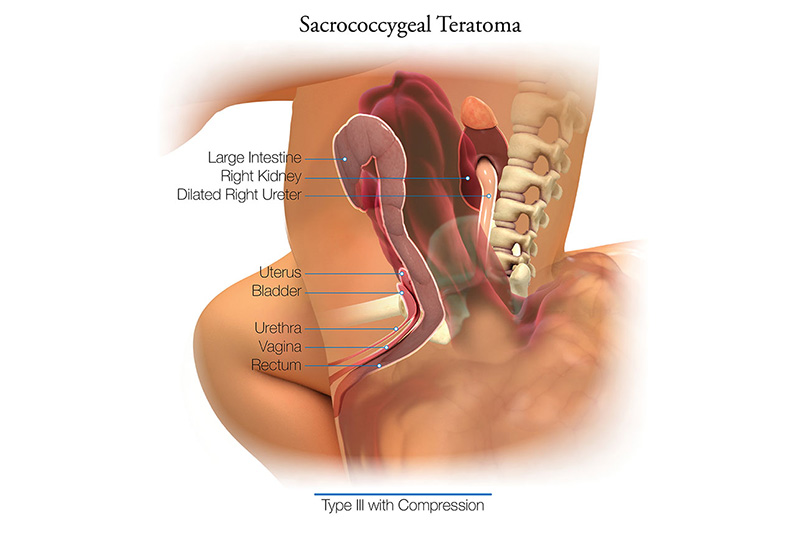
Sacrococcygeal Teratomas
Sacrococcygeal teratoma (SCT) is a tumor that forms on a fetus’ tailbone, also called the coccyx. The tumors are usually not cancerous (benign) but can be life-threatening if not treated. SCT is rare, occurring in about 1 in 35,000-40,000 births. They are more common in males than females.

Myelomeningocele (Spina Bifida)
Spina bifida is a type of neural tube defect, which is a problem with the spinal cord or the structures that cover it. The neural tube normally closes during the early weeks of embryo development, and can occur at any point along the spine (“backbone”). Spina bifida occurs because of the neural tube not closing completely during an unborn baby’s development, causing a hole in some of the bones of the spine (vertebrae). This may result in spinal cord and nerve damage, which may cause mild to severe disabilities.
Click here for a full list of conditions we care for at The Fetal Center.
Contact us directly if you don’t see the condition you are looking for. We welcome the opportunity to talk through your unique medical needs and questions.
Fetal Intervention and Surgery
The Fetal Center at Nationwide Children’s Hospital is one of only a few centers in the nation with expertise to offer a full range of fetal therapies, including fetal intervention and open fetal surgery.
Our expert team evaluates and treats nearly every fetal complication and works collaboratively to recommend the best possible treatment. While many conditions can be managed through noninvasive therapies, some may require fetal intervention or fetal surgery.
The Fetal Center currently offers the following fetal interventions and therapies:
- Open fetal surgery for life-threatening or devastating fetal conditions, including myelomeningocele/spina bifida, sacrococcygeal teratoma (SCT), and congenital lung malformations (CCAM/CPAM)
- Minimally invasive fetoscopic surgery, including:
- laser ablation for twin-to-twin transfusion syndrome (TTTS)
- myelomeningocele (MMC) repair
- amniotic band resection
- fetoscopic treatment for Congenital High Airway Obstruction (CHAOS)
- fetal cystoscopy for lower urinary tract obstruction (LUTO)
- Percutaneous procedures for:
- bladder and chest shunt placement
- Fetal cardiac intervention
- Fetal aortic valvuloplasty
- Balloon atrial septostomy
- Intrauterine blood transfusions
- radiofrequency ablation (RFA) for twin reversed-arterial-perfusion sequence (TRAP)
- bipolar cord coagulation (BCC)
- Amnioreduction
- Amnioinfusion
- Ex utero intrapartum treatment (EXIT) for:
- Congenital high airway obstruction (CHAOS)
- Giant neck or oropharyngeal masses
When fetal intervention is required, procedures are performed at Nationwide Children’s Hospital in a specially equipped operating room. After the procedure, patients are transported to our fetal care unit with a dedicated team of experts for both mom and baby.
If needed, your baby will receive immediate care in our Neonatal Intensive Care Unit (NICU). As a level IV NICU, our staff are experienced in caring for babies who have fetal anomalies and who are critically ill. Nationwide Children’s is home to the largest neonatal network in the country, providing the most comprehensive newborn care in the region.
Babies who have been diagnosed or treated with a congenital heart defect may receive care in the Cardiothoracic Intensive Care Unit (CTICU) which was specially designed for the complex care and needs of pediatric cardiac patients. The dedicated CTICU team is specially trained and equipped to provide the highest level of care to critically ill cardiac patients.
Our Team and Our Partners
Our collaborative team of fetal experts has decades of experience treating all types of fetal conditions and anomalies. Through our collaborative approach to care, we strive to deliver high quality care and best possible outcomes for both fetus and mom.

Adolfo Etchegaray
Adolfo Etchegaray, MD, is the Chief of Fetal Medicine at Nationwide Children’s Hospital. He brings over a decade of experience in maternal-fetal medicine and fetal surgery and years of program development to our Fetal Center. Before joining Nationwide Children’s, Dr. Etchegaray was recruited by the Austral University Hospital in Pilar, Argentina to develop one of the first fetal medicine units in the country. Dr. Etchegaray’s main areas of interest and research are congenital anomalies, fetal therapy, and prenatal screening for chromosomal diseases and preeclampsia.

Oluyinka O. Olutoye
In addition to being the Chief of Surgery at Nationwide Children's, Dr. Olutoye is a pioneer in the surgical and medical treatments that improve outcomes for both mother and baby. As a pediatric and fetal surgeon, Dr. Olutoye brings specialized clinical expertise in fetal and neonatal surgery. Fetal surgeons work closely with obstetricians and maternal-fetal medicine specialists to provide exceptional care for babies who need surgery in-utero and to improve outcomes for a range of conditions such as congenital diaphragmatic hernia, spina bifida and other congenital anomalies.
Susan M. Lopata
Dr. Susan Lopata is the Director for Neonatal-Perinatal Care at the Fetal Center at Nationwide Children’s. Dr. Lopata has developed expertise in delivery room stabilization and care of complex neonates with prenatally diagnosed conditions.

Karen M. Texter
Karen M. Texter, MD, is Director of Fetal Echocardiography at The Heart Center at Nationwide Children's Hospital. Her special interests include echocardiography in congenital and acquired heart disease, and fetal cardiology.

Mickey Johnson
As the Director of Fetal Services, Mickey Johnson, MHA, RN, works closely with all members of the Fetal Center team to support the program's clinical needs. This includes planning, development, implementation, and evaluation of strategies, evidence-based clinical programs, policies, and standards of care. Mickey has over 18 years of progressive health care leadership and over 30 years perinatal nursing experience.

Lisa Miller
As the Clinical Lead and Education Specialist for the Fetal Center, Lisa leads the nursing team supporting fetal unit clinical operations. This includes working closely with the multidisciplinary team to deliver educational and simulation experiences to support seamless care delivery. She is passionate about nursing leadership, staff recognition, patient experience, program development, and evidence-based practice. Lisa received her bachelors degree from Otterbein University and her master’s degree from Mount Carmel College of Nursing.

Christy Stocker
As the Service Line Administrator for The Fetal Center, Christy works closely with all members of The Fetal Center to complete many of the program’s business needs. This includes coordination of the planning, development, implementation, and evaluation of all activities and programs associated with The Fetal Center. In addition to working with this team, Christy is also the Service Line Administrator for Pediatric and Adolescent Gynecology. She has over 20 years of progressive leadership experience. Her background includes a Bachelor of Science in Industrial Engineering and an MBA from the University of Dayton.
Partners in Care
In addition to our dedicated fetal care team, you will have the opportunity to meet with pediatric specialists to learn more about recommended treatment options and follow up care.
Depending on your baby’s diagnosis, you may also meet with the following:
Meet Our Fetal Center Patients
At the Fetal Center at Nationwide Children's, we treat babies even before they're born. When prenatal testing detected a birth defect in their unborn babies, these families came to Nationwide Children’s for support and care. Here are their stories.



Why Choose Nationwide Children's?
The Fetal Center at Nationwide Children’s is one of a kind. It’s a place where world-class clinical care and experts from nationally ranked programs are here to care for you and your unborn baby. Nationwide Children’s Research Institute is on the cutting edge of genetic diagnosis, gene therapy and clinical research, offering access to new groundbreaking treatments.
From the moment you connect with our team, you’ll feel the difference. It’s not just how the care coordinators make you feel at ease, but it’s the way they help you take care of every detail — from insurance questions and scheduling to planning your stay from start to finish. Here are some of the many ways Nationwide Children’s stands apart from other fetal centers across the country.
- Second opinions: If you want a second opinion, the Fetal Center team can help. The team of specialists work together to provide comprehensive feedback on your diagnosis and treatment plan. This can be done through an in-person visit or via an online written report. Our team can help you decide which is right for you.
- A national destination for fetal care: Nationwide Children’s is consistently recognized by U.S. News & World Report for excellence as an institution in all 10 pediatric fields. We are also named an Honor Roll Hospital, a designation awarded to only 10 pediatric hospitals each year.
- Genetic and other advanced testing to diagnose fetal conditions: Clinical (or medical) Genetics is a medical specialty that uses genetic and genomic information to diagnose and treat hereditary disorders. These genetic advancements revolutionize fetal care and can advance care for rare conditions.
- Prenatal and postnatal care for you and your baby: Whether you deliver your baby at Nationwide Children’s or another hospital, your care team is here and ready for you before, during and after pregnancy.
- Maternity care from expert MFMs to ensure mom's safety before, during and after delivery: The Fetal Center includes more than fetal and pediatric experts. We also have the maternal experts to care for mom.
- A dedicated fetal unit equipped for high-risk pregnancies and staffed with a dedicated team: Few fetal and pediatric centers offer the nation’s best subspecialists on the same campus (including neonatology, heart and pediatric surgery). This means your baby’s long-term follow-up care is seamless.
- Fetal cardiac intervention: In a high-risk delivery, every second counts.
- Full range of fetal surgery offerings: There are less than a handful of places in the United States that can offer the full range of fetal surgery and treatments that Nationwide Children’s can. Our hospital is centrally located and easily accessible from across the Midwest. Plus, our surgeons have combined 35+ years of experience.
- Ronald McDonald House: Conveniently located right on our main campus, just steps away from the hospital, the Ronald McDonald House allows you to remain a part of your child’s care team while providing you a home away from home.
- A national and international destination: We’ve treated hundreds of patients from across the United States and around the world. Whether you are traveling from outside the United States or from another state, our Global Patient Services team can help make your trip as seamless as possible.
Becoming a Patient
We understand that this can be a difficult time. At Nationwide Children's, our fetal care team is here to support you and your family every step of the way.
To become a patient or speak with a member of our team, please call (614) 722-BABY.
Physician referrals may be completed by using this form or by printing this form and returning by fax.
Evaluation and Patient Visits
If a fetal concern is detected by your current care team, you may be referred to the fetal center at Nationwide Children’s for additional testing and evaluation. Whether you are coming for a single consultation or being seen several times throughout pregnancy, our goal is to provide you with the information and care you need to prepare for the birth of your baby, as well as what to expect after delivery.
Our nurse coordinators will help schedule all appointments and visits at Nationwide Children’s so you can see all necessary specialists in one day. To help prepare you for the birth and care of your baby, our nurse coordinators will arrange a tour of our Neonatal Intensive Care Unit (NICU) or Cardiothoracic Intensive Care Unit (CTICU) before your baby’s birth. We will also make sure you go home with literature and educational resources to help you understand your care and your baby’s diagnosis.
Your First Visit - What to Expect
Out-of-town Patients
Our team provides compassionate support to all families, whether traveling a few miles or across the globe. Our Global Patient Services, Fetal Center staff and navigators will assist you with any of your family’s housing, transportation, insurance, and scheduling needs.
Inside The Fetal Center
Conditions We Treat
- Abdominal / Duplication Cysts
- Agenesis of the Corpus Callosum
- Amniotic Band Syndrome (ABS)
- Anencephaly
- Aortic Stenosis
- Atrioventricular Septal Defect (AVSD)
- Bilateral Renal Agenesis
- Bladder Exstrophy
- Bladder Outlet Obstruction
- Bronchopulmonary Sequestration (BPS)
- Cervical Teratoma
- Cleft Lip and Palate
- Cloacal Exstrophy
- Clubfoot
- Coarctation of the Aorta
- Congenital Diaphragmatic Hernia
- Congenital Heart Defects
- Congenital High Airway Obstruction Syndrome (CHAOS)
- Congenital Lobar Emphysema
- Congenital Lung Lesions
- Congenital Pulmonary Airway Malformation (CPAM)
- Craniosynostosis
- Cystic Adenomatoid Malformations
- Dandy-Walker Syndrome
- Diaphragmatic Hernia in Children
- Double Outlet Right Ventricle (DORV)
- Down Syndrome (Trisomy 21) in Children
- Duodenal Atresia
- Ectopic Ureterocele
- Encephalocele
- Esophageal Atresia
- Gastroschisis
- Genetic and Metabolic Diseases and Disorders
- Giant Neck Mass
- Hemolytic Disease of the Fetus and Newborn (HDFN)
- Heterotaxy (genetic)
- Hirschsprung Disease
- Hydrocephalus
- Hydronephrosis
- Hydroureter
- Hypoplastic Left Heart Syndrome
- Interrupted Aortic Arch (IAA)
- Lower Urinary Tract Outlet Obstruction (LUTO)
- Micrognathia
- Multicystic Dysplastic Kidney
- Omphalocele
- Pelviectasis
- Pierre Robin Sequence
- Polycystic Kidney Disease (PKD)
- Posterior Urethral Valves
- Pulmonary Atresia
- Pulmonary Atresia with Intact Ventricular Septum (PA/IVS)
- Pulmonary Stenosis
- Pyelectasis
- Renal Agenesis
- Sacrococcygeal Teratoma (SCT)
- Short Bowel Syndrome
- Spina Bifida and Myelomeningocele
- Teratomas
- Tetralogy of Fallot (TOF)
- Total Anomalous Pulmonary Venous Return (TAPVR)
- Tracheoesophageal Fistula (TEF)
- Tracheoesophageal Fistula and Esophageal Atresia
- Transposition of the Great Arteries (TGA)
- Tricuspid Atresia
- Trisomy 13 and Trisomy 18 in Children
- Trisomy 21
- Truncus Arteriosus
- Twin Reversed Arterial Perfusion Sequence (TRAP Sequence)
- Twin-to-Twin Transfusion Syndrome
- Ureteropelvic Junction Obstruction (UPJ Obstruction)
- Ventricular Septal Defect (VSD)
- Ventriculomegaly
- Vesicoureteral Reflux (VUR)
