Duodenal Atresia
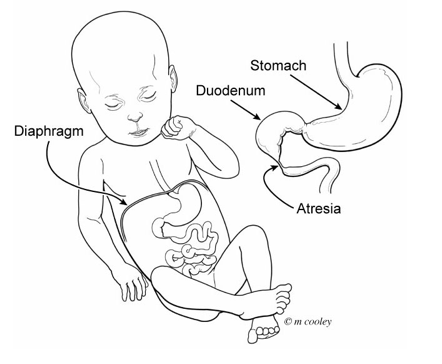
Duodenal atresia is a congenital condition where the duodenum is narrowed or blocked. This blockage keeps liquids and food from passing through the stomach into the rest of the intestine.
What is Duodenal Atresia?
The duodenum is the first part of the small bowel (intestine). It is directly connected to the stomach. Duodenal atresia is when the duodenum is a narrowing or blocked. This blockage keeps liquids and food from passing through the stomach into the rest of the intestine.
What Causes Duodenal Atresia?
The cause of duodenal atresia is not known. It is congenital, meaning it happens before your baby is born. Duodenal atresia happens in 1 out of every 6,000 live births. Babies born with duodenal atresia often have other problems at birth, including heart defects. About 30% of babies with duodenal atresia have Down Syndrome.How is Duodenal Atresia Diagnosed?
Duodenal atresia may be found during routine prenatal ultrasound but sometimes it is diagnosed after the baby is born. If your baby has duodenal atresia, the ultrasound may show fluid in your baby’s stomach and part of the duodenum, but no fluid beyond that. This is called the double-bubble sign. The prenatal ultrasound may also show too much amniotic fluid in your womb. This condition is called polyhydramnios.
If your doctor thinks there is a problem, more tests may be ordered. These may include:
- Fetal echocardiogram: A special ultrasound used by a pediatric heart doctor(cardiologist) to look closely at your baby’s heart and surrounding blood vessels.
- Fetal MRI (magnetic resonance imaging): A non-invasive imaging test to get a clear, more detailed image of your baby’s organs. It may help find other problems your baby may have.
Other Tests
Some congenital conditions are caused by changes in DNA, or a baby’s genetic make-up. The doctors may suggest genetic testing to find out more about your baby’s DNA.
- Cell-Free Fetal DNA testing: A screening test where a sample of your blood is taken to look for copies of fetal (baby) DNA. A positive result means that there could be problems with the baby’s DNA. It should be confirmed with another test. A normal result does not mean that there are no underlying genetic problems. Other testing can be done before or after birth depending on your needs and the needs of the baby. This test can see if your baby has Down Syndrome.
- Amniocentesis: A medical procedure in which a small amount of amniotic fluid is taken and studied to screen for genetic problems. This test is usually done in the middle of the second trimester. An amniocentesis can be used to confirm findings on the cell-free fetal DNA test. This test can diagnose Down Syndrome.
- Testing the baby: After birth, a test is done with a sample of your baby’s blood to look for chromosome problems. This is called either a “karyotype” (basic chromosome study), or microarray ((a more detailed look at smaller sections of DNA).
Care During Your Pregnancy
If a test finds you are carrying a baby with suspected duodenal atresia, you will continue to receive care from your obstetrician. Your obstetrician may refer you to The Fetal Center at Nationwide Children’s. There, you will meet with a multidisciplinary team including:
- neonatologists - doctors who specialize in treating newborns)
- neurosurgeons - doctors who perform brain surgery
- neurologists - doctors who specialize in the brain
- nurses
- nurse coordinators - help answer your questions and concerns, guide you through your pregnancy, and prepare you for what to expect
Your doctor will watch your pregnancy closely. You will deliver your baby at a hospital that is ready to care for high risk babies like yours. You should discuss your plans for labor and delivery with your obstetrician. Contact your doctor right away if you have any concerns.
Care After Your Baby Is Born
At the delivery hospital, the neonatologist will manage the care of your baby. They will assess your baby’s breathing and heart rate and examine the baby for other problems.
- Your baby will receive care in the delivery hospital’s neonatal intensive care unit (NICU)
- A tube will be put into your baby’s nose (nasogastric, NG) or mouth (orogastric, OG) down into your baby’s stomach. This tube helps to drain fluid from the stomach that builds up because of the blockage in the duodenum.
- An intravenous line (IV) will be started in your baby’s belly button, arm, hand, foot or scalp. The IV provides fluids to prevent dehydration and provide nutrition. It can also give antibiotics to prevent infection, if needed.
- Your baby will be transferred to Nationwide Children’s main NICU to continue their care and treatment.
- We strongly encourage you to start pumping breastmilk for your baby right away. While your baby will not be able to take any milk until after surgery, it is important to start pumping to establish your milk supply. Breast milk is best for all babies.
How is Duodenal Atresia Treated?
- Your baby will not be able to drink formula or breast milk until after the intestines have healed from surgery.
- A special IV called a peripherally inserted central venous catheter (PICC) will be used to give your baby IV nutrition called total parenteral nutrition (TPN). TPN has all of the calories and nourishment needed for your baby to grow.
- An X-ray of the chest and abdomen will be taken to look for any other problems.
- Ultrasounds of the heart, kidneys and brain will be done to look for any other problems.
- Genetic testing will be done if it was not completed before birth.
- Babies with Down Syndrome may need more evaluations.
Surgery
Once the baby is stable, they will need surgery. It may be a couple of days after birth, or it may be delayed if your baby has other problems that need to be addressed. While surgery is necessary, it is not needed emergently as long as the baby is getting IV fluids and nutrients and the OG or NG tube keeps the stomach empty. The pediatric surgeon will remove the portion of the duodenum that has the narrowing or blockage and reconnect the healthy ends together. A gastrostomy tube (G-tube) may be placed in the stomach to help provide nutrition. The pediatric surgeon will discuss this with you.
Care After Surgery
After surgery, your baby will continue to receive care in the hospital’s NICU. Your baby will need to be on a breathing machine until they are fully recovered from surgery.
Other treatments your baby will probably need after surgery are:
- Antibiotics to prevent infection
- Fluids and TPN given through the PICC
- Oxygen
- Pain medicines, as needed
- The NG or OG tube will stay in place until your baby’s intestines start working.
This may take several weeks. Your baby will not be able to eat until the intestines have healed.
Feeding
Feedings are started once the intestines are fully healed after surgery. Your baby will be started off with small amounts of breast milk or formula, and the amount will be increased slowly over time. Your baby may be able to take milk by bottle or may need to have feeds given through an NG or OG feeding tube. When your baby is taking enough breast milk or formula to grow and gain weight, the IV or PICC will be removed. If your baby has been receiving milk through a feeding tube, we will help your baby learn to feed, either by bottle or direct breastfeeding. Depending on your baby’s other problems, they may need to go home with a feeding tube.
Problems or complications
- Infection: Your baby may be on antibiotics at birth and for several days after surgery. The surgeon and staff will watch your baby very closely for any signs of infection.
- Sometimes babies need a blood transfusion
- Feeding problems after surgery: It takes several weeks for the intestines to heal properly and can be slow to handle food.
Discharge Planning
You will be able to take your baby home once they are taking enough breast milk or formula to grow and gain weight. The total length of time your baby will stay in the hospital will vary. It will depend on whether your baby is born with other health issues or if there are problems after surgery. The usual length of stay in the hospital is about 3 to 4 weeks.
Looking Ahead
Your baby will need regular follow-up appointments to measure growth, development, and nutrition. You will want to find a local pediatrician to take care of routine checkups, vaccines and doctor’s visits. The program coordinator can help you if needed. The pediatric surgeon will follow up with your baby’s surgical needs for as long as needed.
