Hydrocephalus
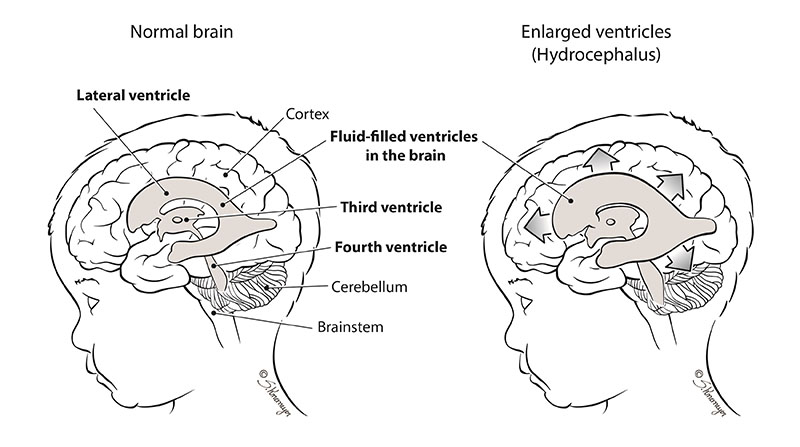
Hydrocephalus occurs when too much fluid builds up inside the spaces around the brain. This fluid, called cerebrospinal fluid (CSF), surrounds and cushions the brain and spinal cord. Hydrocephalus can be caused by a blockage in the flow or reabsorption of CSF, causing extra fluid to build up.
What is Hydrocephalus?
There are several spaces inside and around the brain filled with fluid, called cerebrospinal fluid (CSF). CSF is a clear fluid that surrounds and cushions the brain and spinal cord. CSF is constantly being produced, and must flow through the fluid spaces in order to be reabsorbed. Sometimes, too much fluid can build up inside the spaces, and this a called Hydrocephalus. Hydrocephalus can be caused by a blockage in the flow or reabsorption of CSF, causing extra fluid to build up. On rare occasions, hydrocephalus is caused by the body making too much CSF. The extra buildup of CSF can cause the skull to become larger, can increase the pressure inside the brain, and can be harmful to brain development.
What Causes Hydrocephalus?
Hydrocephalus can be congenital, meaning that it happens before your baby is born. Some reasons for too much cerebral spinal fluid (CSF) in the brain include:
- The flow of cerebral spinal fluid is blocked
- The cerebral spinal fluid does not get absorbed into the blood properly
- The brain makes too much of cerebral spinal fluid
Hydrocephalus can affect the brain and your baby’s development. The extent of the problem depends on the severity of the hydrocephalus, and the presence of other problems such as:
- Genetic defects
- Certain infections during pregnancy
- Bleeding inside the head
- Tumors in the brain or spinal cord
- Injury
- Prematurity
- Abnormalities of brain development
How is Hydrocephalus Diagnosed?
Hydrocephalus may be found during routine prenatal ultrasound but sometimes it is discovered after the baby is born. If your doctor suspects a problem, additional tests may be ordered. These may include:
- Fetal echocardiogram: A fetal echocardiogram is a special ultrasound used by a pediatric heart doctor (cardiologist) to look closely at your baby’s heart and surrounding blood vessels.
- Fetal MRI (magnetic resonance imaging): This type of imaging gives more detailed pictures of your baby’s organs, particularly the brain.
Other Tests
Some congenital conditions are caused by changes in DNA, or a baby’s genetic make-up. The doctors may suggest genetic testing to find out more about your baby’s DNA.
- Cell-Free Fetal DNA testing: Your doctor can take a sample of your blood to look for copies of fetal (baby) DNA. This is only a screening test. A positive result means that there could be problems with the DNA. This should be confirmed with another test to be sure of the result. This additional testing can be done before or after birth depending on your needs and the needs of the baby.
- Amniocentesis: A small sample of the amniotic fluid that surrounds the baby in the womb is taken and tested for DNA problems. This test is usually done in the middle of the second trimester. An amniocentesis can be used to confirm findings on the cell-free fetal DNA test.
- Testing the baby: After birth, a test is done with a sample of your baby’s blood to look for chromosome problems. This is called either a “karyotype” (basic chromosome study), or microarray (a more detailed look at smaller pieces of DNA.
Care After Your Baby Is Born
 At the delivery hospital, a neonatologist (a doctor who specializes in treating newborns) will manage the care of your baby. The neonatologist will assess your baby’s breathing, heart rate, measure the head size, and examine the baby for other problems. Your baby’s head may appear larger than normal.
At the delivery hospital, a neonatologist (a doctor who specializes in treating newborns) will manage the care of your baby. The neonatologist will assess your baby’s breathing, heart rate, measure the head size, and examine the baby for other problems. Your baby’s head may appear larger than normal.
Your baby may have several tests to confirm hydrocephalus and look for the cause. Additional pictures of your baby’s brain will be taken by ultrasound and/or magnetic resonance imaging (MRI), to determine how severe the hydrocephalus is, and whether there are any additional problems with the brain. Additional genetic testing may be needed as well.
Depending on your baby’s condition:
- Your baby may be able to breastfeed or feed from a bottle and then go home with you. It is very important for your baby to follow up with the neurosurgeon in the office for a complete evaluation.
- Your baby may receive care in your delivery hospital’s neonatal intensive care unit (NICU).
- An intravenous line (IV) may be started in your baby’s arm, hand, foot or scalp. The IV provides fluids, medicines, nutrients and antibiotics to prevent dehydration and infection.
- Your baby may be transferred to Nationwide Children’s NICU for further care. If your baby needs additional consultation with other specialists, such as pediatric neurologists (doctors specializing in the brain) or pediatric ophthalmologists (doctors specializing in the eyes), your baby will need to be transferred. Often, the transfer can be delayed until you are discharged from the hospital
How is Hydrocephalus Treated?
If treatment is needed, the goal is to reduce the pressure in the baby’s head and to drain the cerebral spinal fluid (CSF).
Surgery may be needed to treat hydrocephalus. There are two main types of surgical procedures for managing hydrocephalus. Your neurosurgeon with discuss these with you and decide which is best for your baby.
Ventriculo-Peritoneal Shunt (VP Shunt): The neurosurgeon places a mechanical shunting device called a ventriculoperitoneal shunt (VP shunt) in your baby’s head. This shunt helps to drain the extra fluid inside of your baby’s brain and redirects the fluid to another part of your baby’s body such as the abdomen, where it can be absorbed.
Endoscopic Third Ventriculostomy (ETV) with Chorid Plexus Cauterization (CPC): An alternative to shunt placement for the treatment of hydrocephalus in some patients is endoscopic third ventriculostomy (ETV). The procedure creates an additional opening that allows CSF flow out of fluid spaces in the brain through an opening made deep in the floor of the brain. This procedure may be used in place of a shunt when hydrocephalus is caused by certain CSF flow blockages.
In children younger than 1 year old, ETV must be combined with choroid plexus cauterization (CPC). CPC reduces the amount of CSF made in the brain. If you think of hydrocephalus like a blocked sink, the ETV creates a new drain and the CPC slows the amount of water coming from the faucet.
Care After Surgery
After surgery, your baby will receive care in the Neonatal Intensive Care Unit (NICU). Your baby may need to be on a breathing machine until he or she is fully recovered from surgery.
Other treatments your baby will probably need after surgery are:
- Antibiotics to prevent infection
- Fluids and nutrients given through an IV
- Pain medicines as needed
Complications From Shunts
- infection
- bleeding
- malfunction (blockage)
Looking Ahead
Your baby will need regular follow-up appointments to measure growth, development and nutrition. You will want to find a local pediatrician to take care of the routine checkups, immunizations, and doctor’s visits. The program coordinator can help if needed. Your child will need to be seen by the pediatric neurosurgeon to check his growth and development and that the shunt or ETV-CPC is working properly.
