Congenital Diaphragmatic Hernia
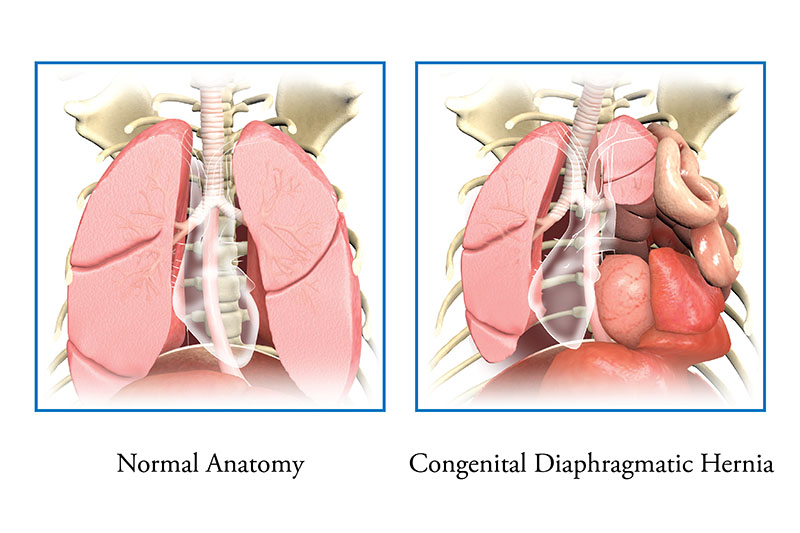
Congenital diaphragmatic hernia (CDH), is a rare congenital condition where the muscles in the diaphragm do not grow together, leaving a hole. The hole allows the intestines and other organs (stomach, liver) to move up into the baby’s chest.
What Is Congenital Diaphragmatic Hernia?
Congenital Diaphragmatic Hernia (di-a-frag-mat-ic), or CDH, is a rare congenital (occurs before birth) condition.
Normally, the diaphragm forms as a thin muscle that separates the chest from the belly. It moves up and down as you breathe to help the lungs fill and empty with air. Typically, the diaphragm is fully formed by the end of the first trimester. In babies with CDH, the muscles in the diaphragm do not grow together, leaving a hole. This can occur on the left or right side of the chest. It is rare that it happens on both sides. 80% of the holes in the diaphragm occur on the left side of the chest. The hole allows the intestines and other organs (stomach, liver) to move up into the baby’s chest. When this happens, it makes it hard for the lungs to grow and develop normally during the rest of pregnancy.
Babies born with CDH can have small, underdeveloped lungs (pulmonary hypoplasia), as well as reduced blood flow to the lungs caused by high blood pressure in the lungs (pulmonary hypertension). These 2 problems, pulmonary hypoplasia and pulmonary hypertension, cause babies with CDH to have a lot of trouble breathing right after birth. Babies with CDH need immediate attention in the delivery room from an experienced neonatal resuscitation team.
What Causes Congenital Diaphragmatic Hernia?
No one knows the exact cause of congenital diaphragmatic hernia. Studies show that 1 in every 2,500-5,000 babies are born with this problem. It is congenital, meaning that it happens before your baby is born. The survival rate is approximately 75%. Survival is usually better when the liver stays in the abdomen.How Is Congenital Diaphragmatic Hernia Diagnosed?
Congenital diaphragmatic hernia may be found during routine prenatal ultrasound. Sometimes is it found after the baby is born. If the condition is suspected, your physician may refer you to a fetal center for a comprehensive evaluation and or order additional testing, including:
- Anatomy ultrasound: a high-resolution ultrasound to confirm the diagnosis and assess for other anomalies.
- Fetal echocardiogram: a specialized ultrasound to evaluate the baby’s heart structure and function.
- Fetal MRI (magnetic resonance imaging): a non-invasive imaging technique to help provide additional details of the baby’s organs that may not have been visualized on ultrasound.
What Are the Symptoms of Congenital Diaphragmatic Hernia?
CDH may not be diagnosed before your child is born. Signs of CDH after birth can include:
- fast breathing or hard breathing (using extra muscles to help breath)
- a very flat belly and “barrel shaped” chest
- cyanosis (bluish color of skin due to low oxygen levels)
Genetic Tests
Some congenital conditions are caused by changes in DNA, or a baby’s genetic make-up. The doctors may suggest genetic testing to find out more about your baby’s DNA. About 30% of babies with CDH may have an underlying genetic problem or syndrome.
- Cell-Free Fetal DNA testing: A screening test where a sample of your blood is taken to look for copies of fetal (baby) DNA. A positive result means that there could be problems with the baby’s DNA. It should be confirmed with another test. A normal result does not mean that there are no underlying genetic problems. Other testing can be done before or after birth depending on your needs and the needs of the baby.
- Amniocentesis: A medical procedure in which a small amount of amniotic fluid is taken and studied to screen for genetic problems. This test is usually done in the middle of the second trimester. An amniocentesis can be used to confirm findings on the cell-free fetal DNA test.
- Testing the baby: After birth, a test is done with a sample of your baby’s blood to look for chromosome problems. This is called either a “karyotype” (basic chromosome study), or microarray (a more detailed look at smaller sections of DNA).
Care During Your Pregnancy
If a test finds you are carrying a baby with congenital diaphragmatic hernia, you will keep getting care from your obstetrician (OB/GYN). Your OB/GYN may also refer you to The Fetal Center at Nationwide Children’s. There, you will meet with a multidisciplinary team including Maternal-Fetal medicine subspecialists, neonatologists (doctors who specialize in treating newborns), pediatric and fetal surgeons (doctors who perform surgery), and nurses to learn more about your baby’s care after they are born. Nurse coordinators will help answer your questions and concerns, guide you through your pregnancy, and prepare you for what to expect.
Your doctor will watch your pregnancy closely. You will deliver your baby at a hospital that is ready to care for high-risk babies like yours. You should discuss your plans for labor and delivery with your OB/GYN. Contact your doctor right away if you have any concerns.
Care After Your Baby is Born
At the delivery hospital, a neonatologist (a doctor who specializes in treating newborns) will manage your baby’s care. The neonatologist will assess your baby’s breathing and heart rate, and examine the baby for other problems.
- Your baby will briefly receive care in your delivery hospital’s neonatal intensive care unit (NICU).
- Your baby will get a breathing tube right after delivery to help them breath. The ventilator is the breathing machine that will provide the lung support.
- A tube will be put through your baby’s nose (nasogastric, NG) or mouth (orogastric, OG) into the stomach. This tube helps to keep the stomach and intestines empty. This reduces pressure of these organs on the lungs.
- Your baby will get a special IVs in their umbilical cord, wrist, or foot. The IVs are used to watch blood pressure and provide medicines. This includes fluids to prevent dehydration, and medicines to prevent infection, help sedate your baby and support blood pressure.
- Your baby will be transferred right away to the Nationwide Children’s Hospital neonatal intensive care unit (NICU) for their care.
- We strongly encourage you to start pumping breastmilk for your baby right away. While your baby will not be able to take any milk until after surgery, it is important to start pumping to establish your milk supply.
Breastmilk is best for all babies.
How Is Congenital Diaphragmatic Hernia Treated?

For more severe cases, your doctor might suggest a surgery called fetoscopic endoluminal tracheal occlusion (FETO). This is done before the baby is born. The surgeon makes a small cut (incision) in the mom’s belly and uterus. They guide a small tool (instrument) and insert a balloon into the baby’s windpipe (trachea). The balloon is inflated with fluid to block (occlude) the trachea. While in utero, the placenta provides oxygen for your baby. The balloon does not affect the baby’s breathing before birth. A second procedure removes the balloon later in your pregnancy. The baby’s lungs can continue to grow and mature before birth. Once your baby is born, surgery will close the hole in the diaphragm.
All babies with CDH will need surgery after birth, but surgery may not be done right away. It is very important to make sure the baby’s breathing is stable and manage the high blood pressure in the lungs before going to surgery. Surgery may be done as early as 2 to 3 days after birth, or as late at 4 to 6 weeks after birth. It is typically done 1 to 2 weeks after birth.
- There are a few medicines your baby’s doctor may use to try and lower blood pressure in the lungs.
- Sometimes babies need a blood transfusion (a process to give your baby more blood). Blood transfusions can help support blood pressure and help deliver oxygen to the body .
- Ultrasounds of the heart, kidneys and brain will be done to look for any other problems in these organs.
- Babies with diaphragmatic hernia are very sensitive to noise, pain, and easily upset. The medical staff will give medicines to help reduce any pain or discomfort your baby may feel.
- If your baby’s lungs are not working well enough to support the body, a special treatment called extracorporeal membrane oxygenation (ECMO) may be needed. This is a heart-lung bypass machine that is a way to let the baby’s lungs rest and heal for a short time. The doctors and nurses will talk to you about ECMO if it is needed.
- Your baby will not be able to drink breast milk or formula until after their intestines have healed from surgery. A special IV called a peripherally inserted central catheter (PICC) will be used to give your baby IV nutrition, called total parenteral nutrition (TPN). TPN has all of the calories and nourishment needed for your baby to grow.
Surgery
Once the baby is stable, they will have surgery. While surgery is needed, it may not be done for days or weeks. When your baby is ready for surgery, the surgeon will decide the best way to move the intestines back into the belly and close the hole in the diaphragm to keep everything in place. This may involve one larger cut (incision), or several smaller incisions, depending on what the surgeon thinks is safest. If the hole is too big and the surgeon cannot sew the diaphragm together, they may use an artificial patch (such as Gore-Tex®) to close the hole in the diaphragm.
Care After Surgery
After surgery, your baby will keep getting care in the NICU. Your baby will need to be on a breathing machine until they are fully recovered from surgery and they can breathe on their own.
Other treatments your baby will most likely need after surgery are:
- Antibiotic medicine to prevent infection
- Fluids and nutrients through the PICC
- Oxygen. Some babies need to go home with oxygen
- Medicines to support blood pressure in the body and lower blood pressure in the lungs
- Pain medicines as needed
- A chest tube to help drain fluid from the incision.
- The NG or OG tube will stay in place until your baby’s intestines begin to work properly. This may take a few weeks. Your baby will not be able to eat by mouth until the intestines have healed.
- The breathing tube will stay in place until the lungs are working well enough to support the baby breathing on their own. Often babies will need continuous positive airway pressure (CPAP) after the breathing tube is removed. CPAP provides high flow air and oxygen through a nose mask to keep the lungs inflated. If your baby is not able to come off of the ventilator, a tracheostomy tube (trach) may be needed to provide longer term ventilator support.
Feedings
Feedings are started once the intestines are fully healed. It may take a few weeks for the intestines to heal and start to work. Often your baby will be fed first through their feeding tube. Your baby will be started off with small amounts of breast milk or formula, and the amount will be increased slowly. When your baby is taking enough breast milk or formula to grow and gain weight, the PICC line will be removed.
Babies cannot breastfeed or take bottles until they are:
- off the ventilator or CPAP
- require low amounts of oxygen flow by nasal cannula. It may take your baby some time to learn how to breastfeed or bottle feed. This is normal.
Your baby can keep getting food though the NG tube while they learn this skill.
Some babies with CDH, especially those with the sickest lungs, may need a long-term feeding tube called a gastrostomy tube (G-tube). This tube is placed through the wall of the belly into the stomach during a surgery. Some babies need to go home with this type of tube.
Risk
Sometimes, even though the doctors and nurses do everything they can, the baby’s lungs are too small and underdeveloped for the baby to live. Unfortunately, despite the doctors and nurses best care, about 2 or 3 out of 10 babies with CDH die in the newborn period. The medical staff will always keep you informed about your baby’s condition and are available to answer any questions or concerns.
Discharge Planning
The total length of time your baby will stay in the hospital will vary. It depends on whether your baby is born with other health issues or if there are problems after surgery. Your baby may be in the hospital for a few months or more depending on their recovery.
Follow-Up
Your baby will need regular follow-up visits with the team to measure growth, development, and nutrition. You will want to find a local pediatrician to take care of all the routine checkups, vaccines and doctor’s visits. The program coordinator can help you if needed. You will also need to follow up with your surgeon, and the neonatal follow up clinic. If your baby goes home with a feeding tube or oxygen, they may need follow up more often.
Long-Term Care
Babies with CDH are at risk for ongoing problems with the lungs, including asthma and respiratory infections. They are also at risk for ongoing problems with feeding, gastrointestinal reflux, and developmental delays. These risks are higher in babies that need ECMO. Physical and occupation therapy and early intervention may be needed to help your child.
Your baby’s hernia may recur. This is especially common with those that require a patch. In this case, they may need more surgery in the future.
CHERUBS (Support Group): CHERUBS was formed to help families of babies born with Congenital Diaphragmatic Hernia. They provide support services, promote research and raise awareness.
