Gastroschisis
![]()
Gastroschisis (gas tro SKEE sis) is a defect in the abdominal (belly) wall. The defect forms before the baby is born. Part of the intestine is outside of the baby's body, rather than inside the abdomen.
The outside of the intestine may be thick and irritated from being exposed to the amniotic (am nee AH tik) fluid that surrounds the baby before birth. Sometimes areas of the intestines are blocked. Often the baby's abdominal space is small for his or her overall body size.
Treatment of Gastroschisis
- If the defect is small, surgery may be done right away to put the intestines inside the abdomen. The muscle and skin will also be closed. This is called a primary closure.
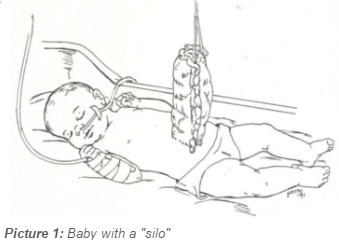
- If the defect is large, closing the skin right away may stretch it too much and may cause too much pressure in the baby's belly. This could make it hard for your baby to breathe if the intestines press against the lungs. Instead, a "silo" or sterile bag will be used for the intestines.
- A plastic material is wrapped around the intestines outside the body. The silo is supported over the baby's belly (see Picture 1). Each day a part of the intestines is gently pushed into the abdomen until everything is inside. In this way, the intestines arrange themselves inside more naturally and the abdominal space stretches a little each day. This is called a staged repair.
- Your baby will receive antibiotics and nutrients (such as sugar, water, electrolytes, protein and fats) through an IV. This is called TPN feeding (Total Parenteral Nutrition). Your baby will not be fed into the stomach until quite a while after surgery. This gives the intestines time to heal. A tube that goes from the nose or mouth into the stomach (called a NasoGastric or OroGastric tube, or NG or OG tube), will help keep the stomach empty.
- Though your baby cannot be fed by mouth during this time, you should give your baby a pacifier. This helps to satisfy your baby's need for sucking.
After the Surgery
- Your baby may be on a ventilator (a machine that makes breathing easier), until he can breathe well on his own.
- All of your child’s nutrients will be given through the IV. He will have an NG or OG (nose or mouth tube) in place until shortly before he begins to be fed by mouth or feeding tube.
- When your baby can take liquids, he or she may be fed by bottle or through a feeding tube. Feedings will be started slowly until your baby’s body can handle more. This is often a slow process.
- Before your baby can go home, he or she must be eating enough formula or breast milk to gain weight normally. This is usually a slow process, and can be frustrating for you and your family. The doctor may need to try several different formulas before finding the one that is right for your child.
- How long a baby will stay in the hospital will depend on many things, including the size and severity of the defect.
- In some cases, the surgeon can close only the skin, and not the muscle underneath. If this happens, another surgery will be needed later after the baby has grown a little more.
- Your baby's hearing will be checked before he or she goes home.
Follow-up Appointments
- You will have a follow-up appointment with the surgeon, usually about 2 weeks after going home. A case manager will arrange this appointment for you.
- You will also need to make appointments with your child’s primary care doctor for regular follow-up care.
Parenting
- We encourage you to touch and hold your baby. The nurses will help and soon you will feel comfortable holding your child.
- You may also bathe your baby and change the diapers. Save them for the nurses to check.
- You may bring toys, music boxes or other items from home to entertain your baby.
This is a stressful time for you, your baby, family and friends. Your doctor, nurses and others are here to help you. If you have any questions, be sure to ask your doctor or nurse.
HH-I-151 Revised 01/15 Copyright 1992, Nationwide Children’s Hospital
