Twin-to-Twin Transfusion Syndrome
Identical twins who share one placenta may be at risk for Twin-to-Twin Transfusion Syndrome, or TTTS. This single placenta contains blood vessels going from one baby to the other. This is usually balanced but is unbalanced in the setting of TTTS.
What is Twin-to-Twin Transfusion Syndrome?
Twins can be either fraternal or identical. Most are fraternal twins — each develops from a separate egg and sperm.
Fraternal twins each have their own placentas and amniotic sacs. Because each twin develops from a different egg and a different sperm, these twins may not look alike. Fraternal twins can be boys, girls, or one of each.
Identical twins are rarer. Identical twins happen when one fertilized egg splits early in pregnancy and develops into two fetuses. Identical twins may share a placenta, but each baby usually has its own amniotic sac. Identical twins are the same sex.
Identical twins who share one placenta may be at risk for Twin-to-Twin Transfusion Syndrome, or TTTS. This problem happens in about 15% of identical twin pregnancies. This single placenta contains blood vessels going from one baby to the other. This is usually balanced but is unbalanced in the setting of TTTS. In TTTS, blood from the smaller “donor” twin is transferred to the larger “recipient” twin through interconnecting vessels, causing an unequal exchange of blood. The recipient twin is larger and is at risk for heart failure because of receiving too much blood from the donor twin. Too much blood forces the heart to work harder. There will be a large amount of amniotic fluid around this baby. The donor twin is smaller because he or she sends blood to the co-twin. As the disease progresses, the donor will produce so little urine that its bladder may not be seen on ultrasound. The amniotic membrane will wrap around the baby, known as a “stuck” twin. With untreated severe cases of TTTS, the survival rate is less than 10%.
What Causes TTTS?
The exact cause of TTTS is not known. TTTS is not hereditary or genetic. TTTS is an irregularity of the placenta that occurs randomly. It is congenital, meaning that it happens before your baby is born.How is Twin-to-Twin Transfusion Syndrome Diagnosed?
TTTS may be found during routine prenatal ultrasound. If your doctor suspects a problem, additional tests may be ordered. These tests enable your doctors to determine the severity and consequently staging of the TTTS. These tests may include:
- Fetal echocardiogram: A fetal echocardiogram is a special ultrasound used by a pediatric heart doctor (cardiologist) to look closely at your babies’ hearts and surrounding blood vessels.
Ultrasound findings that indicate that the pregnancy needs to be closely followed by a high-risk obstetrician include:
- A single placenta
- The same gender
- A thin, hard to see, dividing membrane
- Size differences in the twins
- Polyhydraminos (excess amniotic fluid) in the sac of one twin
- Oligohydramnios (decreased to no amniotic fluid) in the sac of the other twin
- Fetal MRI: If necessary, an MRI- an additional imaging study, may be needed to detect the presence of injury, suffered as a result of the TTTS, to your babies’ brains.
Care During Your Pregnancy
If a test finds you are carrying a baby with TTTS you will continue to receive care from your obstetrician. If you are referred to The Fetal Center at Nationwide Children’s, you will receive coordinated care from obstetricians who specialize in taking care of pregnancies affected by twin-to-twin transfusion.
A coordinator will guide your care from the moment you are referred, scheduling tests and arranging appointments with specialists based on your needs. The coordinator is available to answer your questions and will serve as your single source of information.
Your doctor will watch your pregnancy closely. You will deliver your baby at a hospital that is ready to care for high-risk babies like yours. You should discuss your plans for labor and delivery with your obstetrician. Contact your doctor right away if you have any concerns.
To monitor for TTTS, ideally, ultrasounds are performed every two weeks to evaluate amniotic fluid volumes in both sacs, urinary bladder assessment in both babies, testing blood flow through various blood vessels in both babies and lastly, every 4 weeks to evaluate growth of both babies.
The severity of TTTS can range from mild to severe. Weekly ultrasound measurements of fluid levels, the function of the fetal hearts, and blood flow through the umbilical cords are used to determine how severe the problem is and if treatment is needed.
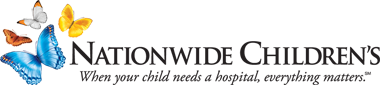
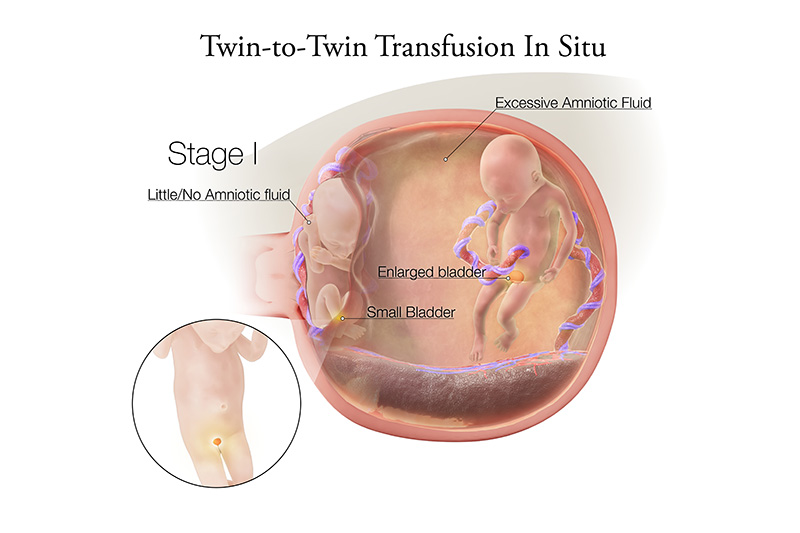
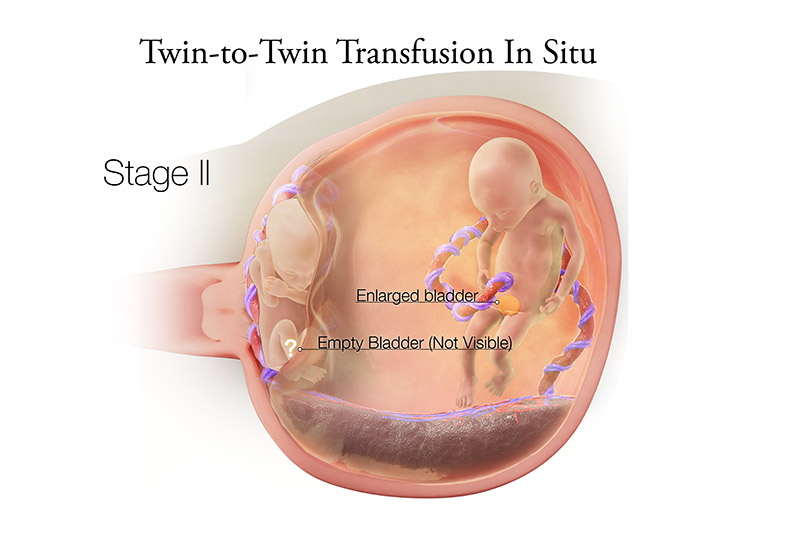
Quintero Staging
Stage I – Significant difference in amniotic fluid levels (recipient measures greater than 8 cm amniotic fluid, donor measures less than 2 cm amniotic fluid). The bladder of the donor twin is visible. Blood flow- Doppler indices (UA, UV and DV) in both twins are normal.
Stage II – Significant difference in amniotic fluid levels persists. However, the donor twin bladder is empty. Blood flow -Doppler indices (UA, UV, and DV) in both twins are normal.
Stage III – Significant difference in amniotic fluid levels and an empty donor bladder persist. However, abnormal blood flow (Doppler indices) is detected: At least one of the following is present in either twin: absent or reversed end-diastolic velocity in the UA, reversed flow in a-wave of the DV, or pulsatile flow in the UV there is abnormal blood flow through blood vessels in the umbilical cord or vessels around the baby’s heart.
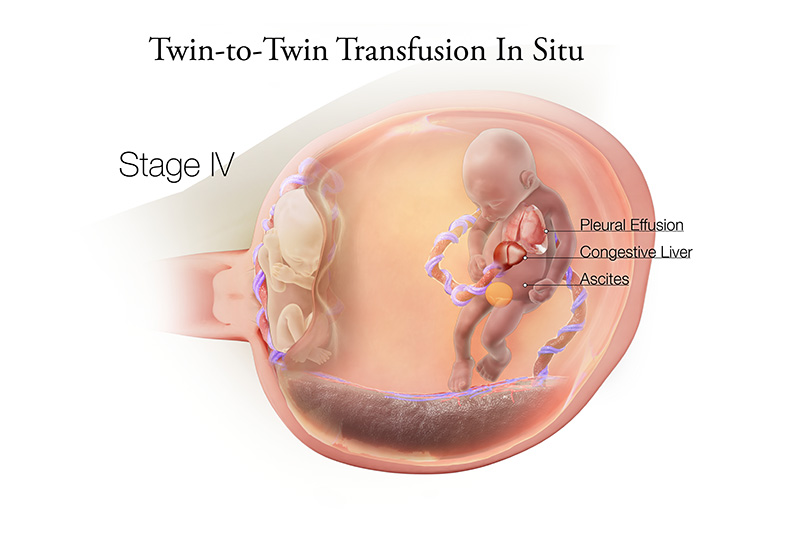
Stage IV – Presence of the above AND fetal hydrops (abnormal fluid accumulation in two out four potential fluid spaces) in one twin
Stage V – Loss of one or both twins
Additionally, you may have warning signs of a sudden increase in the size of the uterus including:
- The sensation of rapid growth
- A uterus that measures large for dates
- Abdominal pain or tightness, or uterine contractions
- Sudden increase in body weight
How is TTTS Treated?
Bed rest may be suggested as a treatment, but has not been scientifically proven to be beneficial. In general however, treatment depends on the gestational age and severity of TTTS. Expectant management for less severe cases and selective Laser photocoagulation (SFLP) for more severe cases.
- There is no scientific evidence that nutritional supplements such as Ensure or Boost help in the treatment of TTTS, but many patients use them because they do not pose much risk as long as you continue to drink other liquids and eat a healthy diet.
- Amnioreduction removes excess amniotic fluid with a thin needle. Because this approach does not treat the underlying cause of TTTS, excess amniotic fluid may recur, resulting in the need for multiple amnioreductions.
- Septostomy uses a needle to make very small holes in the membrane separating the twins, so the amniotic fluid will equalize. This is the least common treatment, but it has been found to decrease the total number of amnioreduction treatments needed during the pregnancy. Both serial amnioreduction and septostomy are not without their limitations compared to the standard of care treatment, Selective laser photocoagulation of placental vessels.
- Laser photocoagulation of the placental vessels uses laser energy to interrupt connecting blood vessels on the surface of the placenta, allowing each fetus to have their individual blood supply. This procedure interrupts the flow of blood from one twin to the other, eliminating the syndrome. This surgery is only performed at certain fetal centers in the US, and you may be referred to one of these locations. This procedure has the most risk, but studies show it is most effective in treating the cause of the disease.
Ongoing Care During Your Pregnancy
Following treatment, weekly ultrasounds of these twin pregnancies are recommended until delivery. In addition to the care for TTTS by a high-risk obstetrician, regular visits to a local obstetrician are needed for routine prenatal care.
Families who are carrying twins with TTTS may face difficult decisions. This disease can change quickly and without warning. Doctors have some ways to measure how the babies are doing, but sometimes the outcomes and timing of upcoming events are unpredictable.
The goal of treatment is to get both babies to an age where they can live outside their mother (at least 28 weeks in general) and be cared for in a neonatal intensive care unit (NICU). In the best situation, where the treatments have been effective or the disease is less severe, these pregnancies are delivered at 34 to 36 weeks.
Your doctor will discuss whether a vaginal or cesarean section delivery is best for you and your babies. This may not be decided until just before the delivery.
Care After the Birth
After birth, treatment depends on the infants’ gestational age at birth and their specific needs. Typically, issues of prematurity determine how much care the babies will need.
All parents ask if one baby is more at risk than the other, while in the uterus or after birth. The answer is that both are at risk for different reasons. The risks for the recipient baby are related to having too much blood flow and fluid. The donor baby’s risks are from having too little fluid and blood flow.
Looking Ahead
After delivery, you will want to find a local pediatrician to take care of routine checkups and immunizations, and to measure growth, development and nutrition.
The nurse coordinator can help if needed.