ECMO (Extracorporeal Membrane Oxygenation)
![]()
ECMO stands for Extracorporeal Membrane Oxygenation. It is a type of life support that uses a machine to pump blood rich in oxygen to support the heart or lungs, or both. The ECMO machine acts as an artificial heart and lung for a patient whose own heart or lungs cannot provide enough blood flow or get enough oxygen into the blood. ECMO is used after other methods of supporting the heart and lungs did not work. Once a patient is on ECMO, you may see an improvement because their heart and lungs may "rest" while ECMO takes over. The goal of ECMO is to let the heart and lungs recover while the patient is supported by the ECMO machine.
Tests before Using ECMO

Some heart defects can cause symptoms that seem at first to be a lung problem. So, before using ECMO, doctors do tests to see if the cause of the problem is the heart or the lungs. It is important to know if the heart is working well or not.
These tests are done before ECMO is started and sometimes at other times during the ECMO course:
- Echocardiogram ("heart echo") uses sound waves to look at the heart’s structure and function. See Helping Hand HH-III-114, Echocardiogram: Sedated.
- Electrocardiogram (EKG) is a test that looks at the heart's electrical system. Please see Helping Hand HH-III-6, Electrocardiogram.
- Ultrasound scan of the head may be done on newborn or very young infants to look for bleeding into the brain. If there is severe bleeding, ECMO may not be used. Please see Helping Hand HH-III-54, Ultrasound Scan.
- CT scan is used when the skulls of older children and adults will not allow the ultrasound waves to be used. Please see Helping Hand HH-III-19, CT Scan.
Access Needed For ECMO
One to three cannulas (tubes) are needed to connect the ECMO circuit to a patient. The surgeon will make a small cut, usually on the right side of the neck. A tube is usually placed through the small cut on the right side of the neck, into the jugular vein. This vein leads to the upper right chamber (right atrium) of the heart (Picture 1, page 1). A second tube is sometimes placed through the same small cut into the carotid artery, another vessel in the neck. These tubes are then connected to the ECMO machine. After the procedure, the blood vessels that are used for this may be permanently tied off and cannot be used in the future. There are 3 other arteries and 3 other veins in the neck that usually continue to supply the brain with blood and oxygen.
Sometimes other sites may be used. For some patients the tubes are placed directly into the heart (right atrium) and into the large artery coming from the heart (aorta). These tubes are then connected to the ECMO machine. These blood vessels are not tied off, and are repaired after the ECMO course.
Types of ECMO
There are different kinds of support that ECMO can provide. Some patients are placed on ECMO to only support their lungs, known as veno-venous ECMO (VV ECMO). This type of ECMO does not support the heart, but is intended to let the lungs rest. If a child is placed on ECMO to support only the lungs, the blood is taken out of the right side of the heart (right atrium), oxygen is added and the blood is returned to the right atrium where the heart then pumps this blood to the lungs and body.
Other patients are placed on ECMO to support their heart and lungs, known as veno-arterial ECMO (VA ECMO). If a child is placed on ECMO to support the heart, the blood is taken out of a vein and returned to an artery.
How ECMO Works
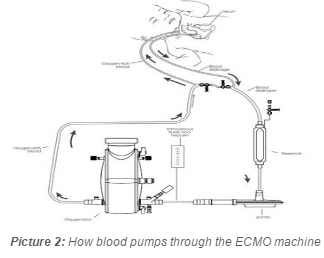
The ECMO machine drains blood from the tube in the jugular vein to the ECMO machine (Picture 2). The ECMO machine can then pump the blood. The blood is pumped through an artificial lung called an oxygenator. This puts oxygen into the blood and takes carbon dioxide (waste gas) out of the blood. The blood is warmed to body temperature as it flows through the heat exchanger within the oxygenator (Picture 2). Blood that is rich with oxygen is then returned through the tube in either the carotid artery or jugular vein.
The blood coming from the child will be dark red (with little oxygen). The blood going back will usually be a brighter red (with oxygen).
Visiting
- You may visit, touch and talk to someone on ECMO, but you will not be able to hold him or her during ECMO therapy.
- You will be given special instructions on hand washing.
- You may be asked to wear a gown over your clothes. This may be to protect the patient from infection or to protect you from getting an infection.
- Parents and grandparents may visit anytime.
- If an emergency occurs with the patient on ECMO or another patient in the unit, you may be asked to leave for a period of time.
- If you are unable to visit, please call anytime.
Medicines
- Heparin (HEH par in) or a similar medicine is given to keep blood from clotting in the tubes while a patient is on ECMO. Antibiotics may also be given to treat infection.
- Pain medicine or a sedative may be given. These medicines are used because we want to keep patients as comfortable as possible while on ECMO. Older children and adults tell us they are almost pain free while on ECMO. Some patients may also be given medicine to keep them from moving to help us keep the tubes as straight as possible and allow the machine to work well.
Blood Administration during ECMO
During ECMO, we will be giving blood products through the ECMO circuit. Blood is given to replace the blood taken for laboratory tests. Platelets (the part of the blood that helps with clotting) are given often to help prevent bleeding. Please see Helping Hand HH-II-122, Blood Transfusion.
Nutrition
ECMO patients usually receive intravenous (IV) fluids for nutrition. Feedings through a tube (placed in the mouth or nose which goes to the stomach) may be started while on ECMO. Some patients will be allowed to eat regular food while on ECMO. After ECMO, regular feedings will be started as soon as possible. As the patient gets stronger, he or she can start taking a bottle, breast-feeding or eating a regular diet as tolerated and ordered by the physician.
Tests Done during ECMO Therapy
- An ultrasound scan of the head may be done on each of the first 3 days while the child is on ECMO and then as needed after that to watch for any bleeding into the brain.
- Chest X-rays will be done daily to check for changes in the lung and to check for changes in the position of the ECMO tubes. The lungs may improve faster than the chest X-rays show. This is because X-rays do not always pick up signs of improvement right away.
- Blood gas labs check the amount of oxygen in the blood. A small sample of blood is drawn from the arterial line. Oxygen and carbon dioxide levels are then measured. This allows us to make the needed adjustments to the ECMO machine and ventilator (breathing machine).
- A small amount of blood will be taken from the ECMO circuit every hour to check the blood clotting time. The heparin or anticoagulant dose may then be adjusted to prevent blood clots. In rare cases, a patient may develop severe bleeding as a result of heparin and will need to be taken off ECMO.
Response to Treatment
The time each patient is on ECMO varies. The amount of time depends on each child’s ability to recover from the underlying illness that required the use of ECMO.
There are several ways to know if there is improvement:
- Chest X-rays will help to show how much the lungs are improving.
- As the heart and lungs or both improve, the doctor may decrease the blood flow through the ECMO machine.
- When the blood flow is decreased, if the blood gas oxygen level stays the same it is usually a sign that the lungs are improving and can now work better on their own.
If the child has not improved after 3 to 4 weeks of ECMO, it may mean the heart or lung disease cannot be reversed. Sometimes, a lung biopsy (taking a tiny piece of lung tissue to look at under a microscope) or a cardiac catheterization is needed. These tests can give more information about the heart or lung disease. Please see Helping Hand HH-III-3, Cardiac Catheterization.
If the medical team agrees that ECMO can no longer be expected to bring about a cure, the patient may be taken off ECMO. Other medical therapy will then be started. The doctors will always discuss these options with you before decisions are made.
Weaning from ECMO
To wean means to slowly readjust back to normal.
- As the heart and lungs become healthier and deliver more oxygen on their own, blood flow through the ECMO machine will be decreased and ventilator support will be increased.
- When a patient can support himself or herself with only a little help from the ventilator, the surgeon will remove the ECMO tubes.
- The incisions will be closed with stitches and covered with a bandage.
- The small scar will fade with time but will not go away completely.
- Then we will begin slowly weaning the ventilator.
Follow-Up Care

- For pediatric patients, we will arrange for you to see a specialist in child development. The specialist and your pediatrician can follow your child's progress after he goes home.
- For neonatal patients, a follow-up visit will be scheduled in 4 to 6 weeks with the Neonatal Developmental Follow-Up Clinic.
- For all children, a developmental specialist will test the child's growth and development skills at 6 months and then from time to time up to at least 5 years of age. Other visits may be needed if there are other medical problems.
- It is important that your child receives follow-up care.
- Be sure to keep all your appointments with the follow up physicians.
If you have any questions, be sure to ask your doctor or nurse
HH-II-90 11/90, Revised 2/18 Copyright 1990, Nationwide Children's Hospital
