Sclerotherapy of Orbital Slow Flow Malformations: A 15 year Single Center Experience
Authors
Purpose
- Present our core techniques for sclerotherapy of orbital slow-flow malformations
- Present our 15 year experience with sclerotherapy of orbital slow-flow vascular malformations
- Encourage awareness of sclerotherapy as an excellent treatment option for these patients
Introduction
Lymphatic and venous malformations (LMs and VMs) of the orbit are benign neoplastic growths that often present during childhood. Although uncommon, they cause lifestyle-limiting symptoms of recurrent pain, swelling, and weeping. They pose a significant risk to vision and can be cosmetically quite deforming. They are very challenging to treat surgically. They are usually lymphatic but can be venous or mixtures of both types of vessels which have been called Veno-Lymphatic Malformations (VLMs). Percutaneous sclerotherapy has previously been shown to be a safe and effective treatment. As a Destination Medical Center for this particular disease we have gained experience with sclerotherapy of these lesions and hope to share some of that in this Tōster.
Methods
Techniques for orbital sclerotherapy

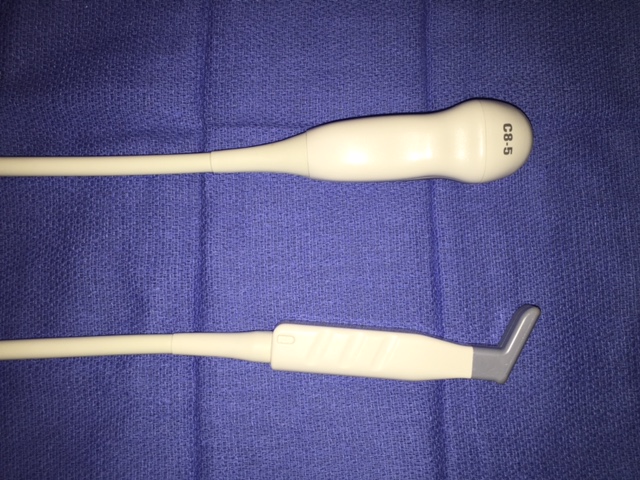

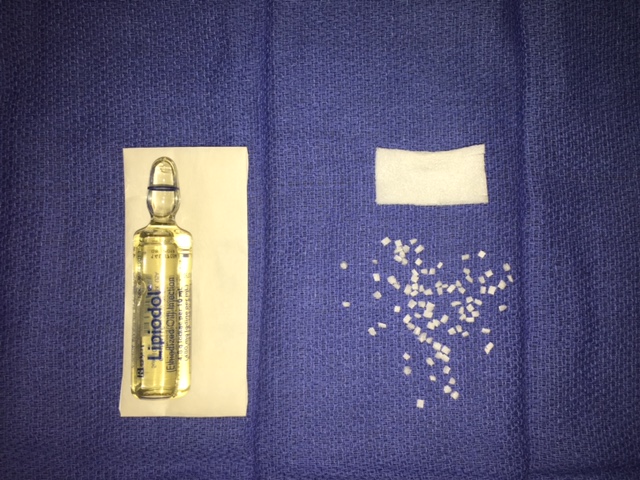
The materials needed are ubiquitous. One needs two different Ultrasound (US) probes for deep and surface disease, medications such as Sodium Tetradecyl Sulfate (STS), Ethanol, Doxycycline (Doxy), and Bleomycin (Bleo). These agents can often be made into foams for injection, with different mixtures of Albumin, Gel Foam Confetti, Ethiodol, and air. The foam increases dwell time of the sclerosant within the lesion and makes the injected material exquisitely easy to see with US, fluoroscopy, or even CT during injection. Mixtures vary depending upon what you are trying to treat and most importantly physician skill with the different agents and imaging modalities. Similar to treatments in other parts of the body, we use US for all needle placements, US for monitoring injections of LMs, and fluoroscopy for monitoring injections of VMs.

The obligatory surgical skill needed for success is the ability to safely and accurately puncture malformations around and behind the globe. Placing needles accurately within the target without mechanically or chemically injuring fragile and important adjacent structures is critical to procedural success and avoiding complications.
For large cysts, a catheter can be placed entirely within the cyst to completely decompress it and temporarily fill it with sclerosant(s) that will be entirely aspirated prior to the end of the procedure.
For smaller cysts and even relatively solid disease it is better to aspirate with a small needle and then inject an agent such as Doxy or Bleo foam that you intend to leave in the lesion.
Sometimes the lesion is completely hidden behind the equator of the globe but is visible with US using the globe as an acoustic window. In this circumstance, it is often helpful to simply bend the needle to the angle needed. This allows you place the needle along side the globe, rotate the needle, and then use the angle of the pre-bent needle to direct its advance into the portions of the lesion behind the globe.
Once safely accessed, aspiration of lymph or blood will confirm needle or catheter position. When treating a large LM cyst with a catheter, the lesion is completely aspirated, a small contrast cystogram is performed to exclude cyst rupture, and then sclerosant(s) are injected and allowed to dwell in the cyst for a short time before complete aspiration. In our practice, these cysts are treated with a small amount of STS for 5 minutes followed by Ethanol for 15-20 minutes. We keep the catheter to bulb suction for 48 hours prior to removal, as very caustic agents will stimulate fluid generation. Lacking a catheter for decompression this can lead to significant swelling behind the globe.
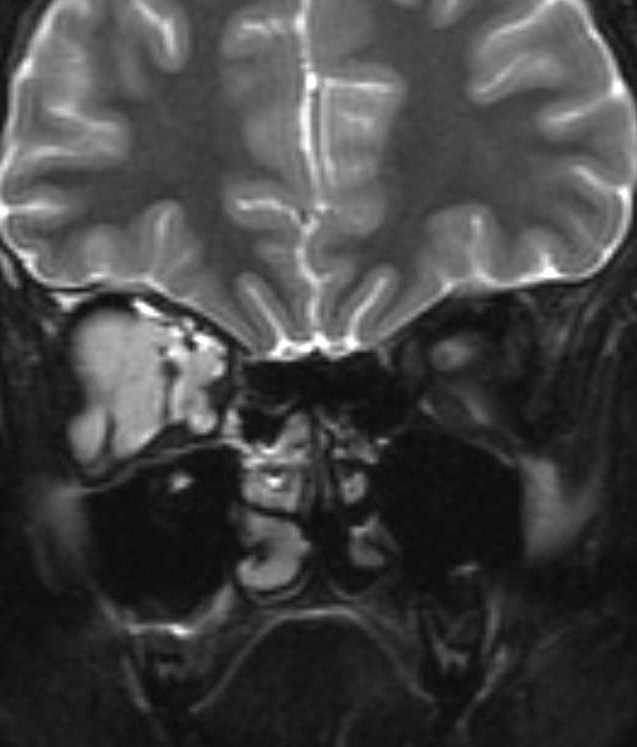

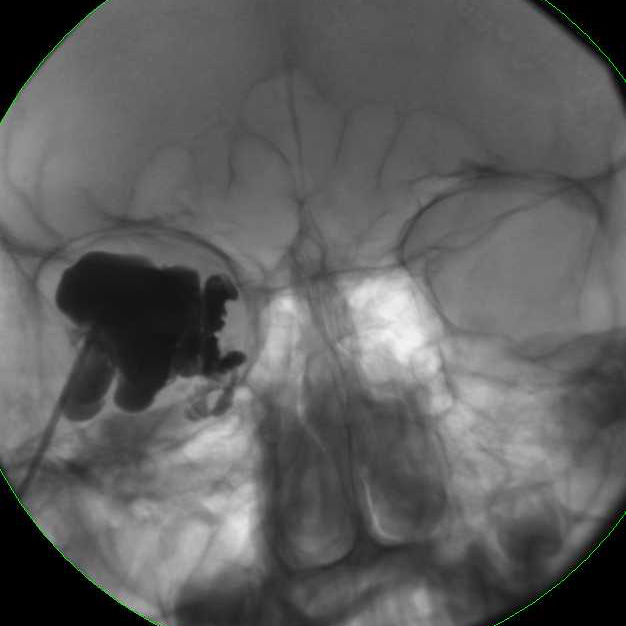
MRI of large LM cyst (top), catheter passing through lower lid (left), cystogram (right).
When treating small LM cysts, US guided injection can be performed slowly and in a controlled way watching the agent in real time spread through a geographic area of the lesion. Often multiple needle punctures will be needed to fill a lesion. We use this technique for injection of Doxy and Bleo foams.

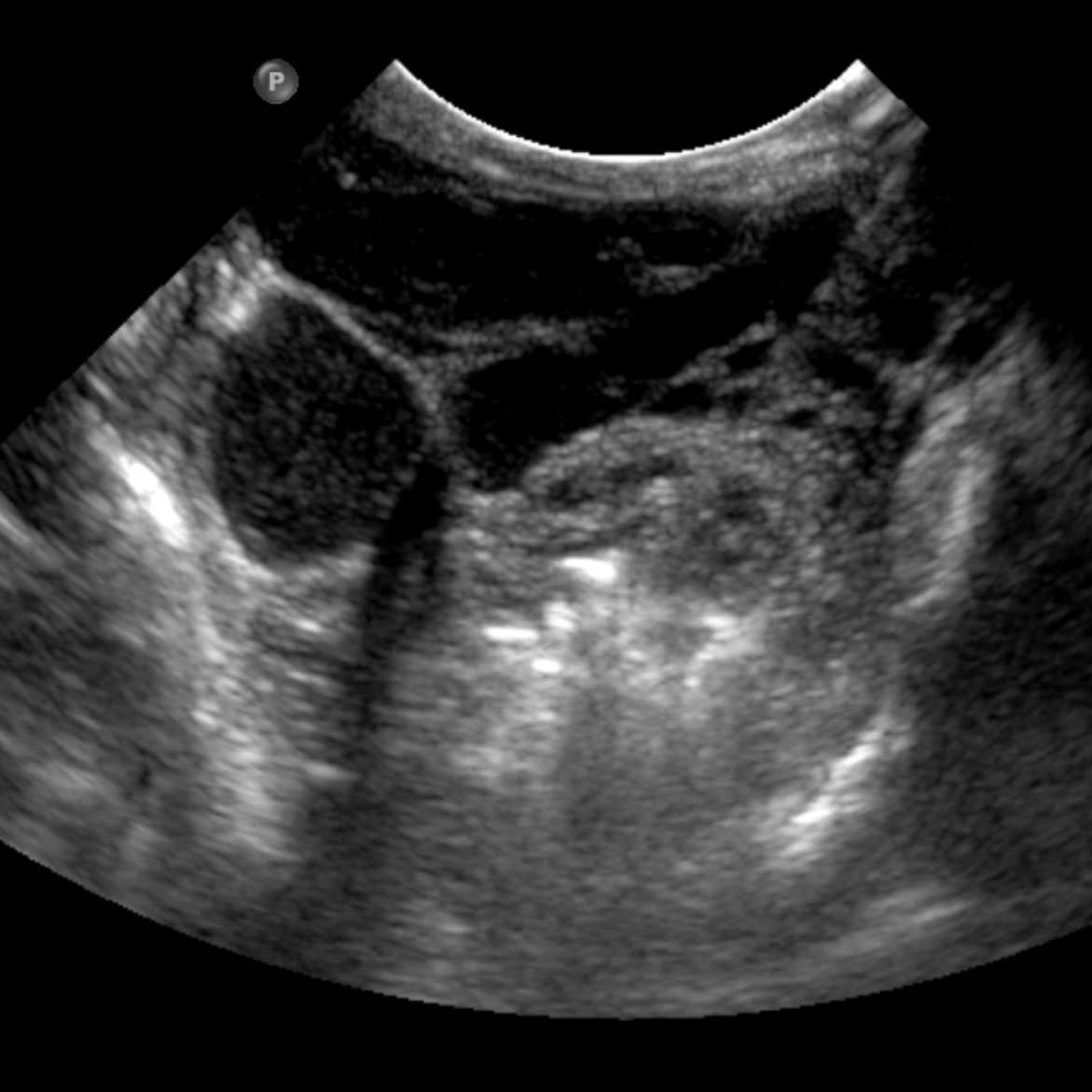

MRI of small LM cysts (top), US of needle injecting individual cysts (left), photo of US guided technique for small cyst puncture (right).
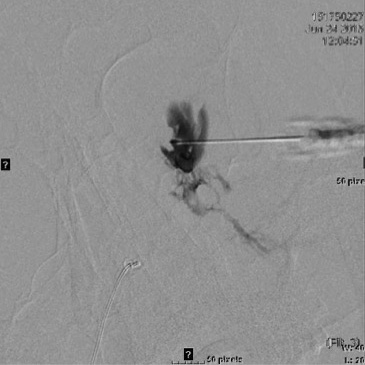
If treating a VM, as in treating a VM anywhere else in the body, a venogram under fluoroscopy is useful to assess the size of the lesion, the routes of venous drainage, and the rate of run off. Using standard fluoroscopic guided sclerosant injection techniques, the foams are all very well visualized especially under subtraction technique.



Video during sclerotherapy procedure to treat an orbital microcystic LM in a child.
Retrospective Review of Outcomes (2000-2015)
- 91 patients were treated during the study period, with 72 meeting the inclusion criteria. As a Destination Medical Center with patients coming from all over the world it is often difficult to get reproducible objective clinical follow up on all patients. Often, even with just one treatment, the patients get enough relief and never need to return so we simply cannot get good ophthalmologic measures of outcome. This study is limited to patients who returned for multiple treatments and reproducible clinical measures could be obtained.
- 27 patients had LMs (37.5%), 32 had VLMs (44.4%) and 13 had purely VMs (18%).
- Which agent and what volumes were injected were at the discretion of the treating physician based upon standard sclerotherapy practices. Sometimes additional areas of facial involvement were treated in the same setting.
- Length of follow up, agent and technique used, number of treatments, recurrence rates during follow up, change in proptosis, and change in visual acuity (VA) were recorded.
Results, Conclusions and References






- 72 patients (32M:40F) with an average age of 13 years (SD ±12) were included in this review
- Average number of treatments was 2.6 (SD ±0.8) for LMs, 3.8 (SD ±1.5) for VLMs, and 3.5 (SD ±2.1) for VMs. As would be expected, lesions with venous components were harder to treat with VLMs getting more treatments than LMs (p = 0.006)
- A total of 236 treatments were performed in the 72 patients using catheter drainage and STS/Ethanol ablation 24 times, Doxy injection 71 times, and Bleo injection 141 times. Treatments have evolved over the nearly 2 decades we have been doing this with improvements in medication and technique as well as changes in personnel
- Average follow-up time was 52.1 months (range 1-146, SD ±23.6)
- 4 patients (5.6%) experienced recurrence during the follow-up time period. 3 recurrences were detected with imaging with only 1 having both clinical and imaging recurrence
- 23 patients had reliable pre and post-procedural exophthalmometry. Of these, 19 had baseline proptosis (82.6%). In no case did proptosis increase and it decreased for nearly all patients.
- 37 patients had Snellen Visual Acuity (VA) readings before and after treatment. No patients experienced a decline in VA and 8 experienced an improvement in VA. The average pre-treatment VA was 20/80 (0.60 log MAR) and the average post-treatment VA was 20/25 (logMAR 0.099) (p = 0.009)
- There were no complications in this series
- Representative pre and post treatment clinical images are presented
- Tools and techniques for orbital sclerotherapy are readily available though the procedures can be technically challenging. As with all sclerotherapy, the tools and medications have pros and cons and often will be dictated by availability of tools and skills unique to each treatment center. Our own protocols have changed over the last 2 decades such that fewer treatments are now performed per patient and Bleomycin is the principle agent used with resultant expected decrease in peri-operative swelling
- Percutaneous sclerotherapy is an effective and safe treatment option for orbital slow flow malformations with low long-term recurrence rates after successful ablation
- Sclerotherapy is a good treatment option for these patients but it requires a team of devoted physicians and attention to technical detail.
- Dasgupta R, Fishman SJ. ISSVA Classification. Semin Pediatr Surg. 2014; 23:158-161.
- Hill RH III, Shiels WE, Foster JA, et. al. Percutaneous drainage and ablation as first line therapy for macrocystic and microcystic orbital lymphatic malformations. Ophthal Plast Reconstr Surg. 2012; 28:119-125
- Barnacle AM, Theodorou M, Maling SJ, Abou-Rayyah Y. Sclerotherapy treatment of orbital lymphatic malformations: a large single-centre experience. Br J Ophthalmol. 2016; 100:204-208.



