Lymphatic Malformation
A lymphatic malformation is the result of abnormal formation and development during fetal development of the otherwise normal lymphatic vessels in the body.
What is a Lymphatic Malformation?
A lymphatic malformation is the result of abnormal formation and development during fetal development of the otherwise normal lymphatic vessels in the body. This is usually in one area of the body:
- Neck
- Chest
- Abdomen
- Extremity
Lymphatic malformation is a common vascular malformation, representing approximately five percent of all benign (harmless) tumors. A lymphatic malformation is a lump of tissue containing bubbles of fluid, known medically as “cysts”.
Are There Different Types of Lymphatic Malformations?
There are two main types of lymphatic malformations based on cyst size detected with medical imaging:
- Large cysts (macrocysts) are called "macrocystic"
- Small cysts (microcysts) are called "microcystic"
The size, location and how fast a lymphatic malformation develops determine how it will affect the body. Some lymphatic malformations are visible at birth. Other lymphatic malformation cysts fill up with fluid later in life and may be detected for the first time later in a child’s life.
Minimally-invasive treatments, alternatives to more extensive and potentially deforming surgical procedures, are now offered by:
- Pediatric surgeons
- Otolaryngologists
- Ophthalmologists
- Oculoplastic surgeons
- Neurosurgeons
- Urologists
- Other surgeons
Case Study 1: Lymphatic Malformation of the Neck, Shoulder and Chest

In the first few hours of life, Hayden underwent a CT scan that clearly illustrated for the pediatric surgeon in Kentucky the extent of the mass, previously seen on a prenatal ultrasound.
The mass involved the left neck, shoulder and the entire length of the left chest wall. Surgical mapping indicated extensive surgical removal involving major nerves and vital structures, resulting in an up to 50 percent chance of recurrence.
After consultation with The Lymphatic Malformation Center at Nationwide Children's Hospital, the surgeon decided against operative removal and transferred Hayden to Nationwide Children's for definitive interventional radiological treatment.
Following the five-hour trip from southern Kentucky, Hayden, age 6 months, underwent his first two-hour procedure that ablated more than 95 percent of the lymphatic malfmormation, through a 2 mm opening in the skin.
Hayden came back six months later to complete his second procedure, which only took 60 minutes, and was released to go home with only a Spiderman bandaid for a dressing, and no remaining cysts for treatment.
Case Study 2: Orbital Lymphatic Malformation
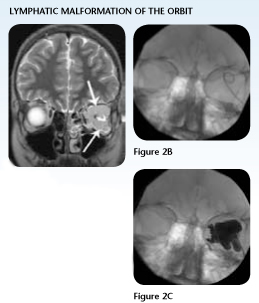
Jordan, age 13, dreamed of being able to do simple things that his friends enjoyed, such as running track, playing baseball and rollerblading, to name a few. Since the age of 3, Jordan had undergone treatment for a left orbital lymphatic malformation.
Each intervention provided little success at relieving his proptosis or recurrent symptoms. By age 13, when his lymphatic malformation flared up, it sent him to the hospital with a severe headache, visual loss and bradycardia.
Surgeons operated to attempt removal of the mass, drained the cystic spaces and consulted with experts around the country for other surgical options. One leading, east coast pediatric teaching center suggested that if additional treatment were attempted, they anticipated Jordan would have a three to four month inpatient stay, and the high risk of recurrence.
Before proceeding with additional surgical options, Jordan's oculoplastic surgeon in Kansas placed his case on the Internet, for fellow oculoplastic surgical opinions around the country. Dr. Kenneth Cahill, Oculoplastic Surgeon at Grant Medical Center and Nationwide Children's Hospital, read the e-mail and recommended that Jordan come to Nationwide Children's for treatment.
Following Dr. Cahill's recommendation, Jordan's surgeon followed up with his family, who opted to make the trip and bring their son to Nationwide Children's Hospital. Jordan needed just one interventional radiology procedure, with a 23-hour inpatient stay.
As a result of the procedure, Jordan no longer has proptosis and has no recurrence of his bradycardia. At age 13, Jordan is realizing his dream of enjoying the simple things. Now his biggest physical complaint is sore leg muscles from running track.
What are the Signs and Symptoms?
Lymphatic malformations can be found in many locations and symptoms can vary. Here we provide basic symptom and diagnosis information. If your child has been diagnosed with a lymphatic malformation, discuss treatment options with your primary care physician.
- Swelling
- Pain
- Bleeding
- Infection (in some cases)
- Visual problems, eye bulging (proptosis) or even blindness (if located in the eye)
Causes of a Lymphatic Malformation
A lymphatic malformation is a result of abnormal development (malformation) of the branching and interconnecting lymphatic ducts, the fluid (yellow fluid) cannot move forward and becomes trapped in small and large bubbles (cysts), which result in a lymphatic malformation. "Yellow blood" travels in lymphatic vessels (channels or ducts). This occurs because the arteries carry red blood cells in liquid to tissues to deliver oxygen. As the red blood cells are squeezed through the tiny capillaries so oxygen can diffuse into body tissues, the "yellow" liquid that carries the red blood cells gets squished from the capillaries into the tissues next to the capillaries.
The lymphatic vessels carry the "yellow blood" from the body tissues back to the heart to mix with the blood from the veins. Blood vessels in the body should be slender tubes that branch, merge into larger tubes downstream, until they reach the large main vein (vena cava) in the body. Lymphatic vessels should also branch (when normally developed) as slender fluid-carrying tubes. With abnormal development, the lymphatic ducts develop incorrectly (lymphatic malformation), and instead of branching vessels, the lymphatic malformation has a cluster of bubbles (cysts) in which the lymphatic fluid (yellow blood) cannot move forward and is trapped in small and large bubbles (cysts).
Diagnosing a Lymphatic Malformation
Ultrasound, MRI or CT scan examinations are commonly used to help diagnose a lymphatic malformation. Definite tissue diagnosis is made with either a surgical biopsy or special, minimally-invasive samples using a small tube placed into the lymphatic malformation to obtain fluid and cells from the walls of the cysts.
More than half are recognized at birth and 90 percent before 2 years of age. Occasionally, lymphatic malformations may first show with a visible mass in early or late adulthood. A lymphatic malformation that is diagnosed at birth usually presents as a soft, spongy, non-tender mass. In older children and adults, a lymphatic malformation may present with rapid development of a firm painful mass, occurring as a result of hemorrhage (bleeding) into previously undiagnosed lymphatic malformation cysts. In this situation, lymphatic malformations may fill up "over night" and be, for the first time, a large painful mass, within hours.
A lymphatic malformation is most frequently diagnosed in the head and neck (including face and tongue), but can show in other locations including the eye (orbit), chest, abdomen, extremities, scrotum and penis.
Lymphatic Malformation Treatment and Procedure Options
Lymphatic malformations are now most often treated using interventional radiology minimally-invasive techniques designed to ablate (or kill) the cysts within the body. In this situation, a chemical injected into the lymphatic malformation cyst kills it. The body then cleans up the dead cyst tissue over time. This can be done without large scars or the need for hospitalization.
In the past, surgical removal has been considered standard treatment for these cavernous lesions, despite recurrences in 15 to 53 percent of reported clinical series. Percutaneous (interventional radiology) treatments for both macrocystic and microcystic lymphatic malformation now offer patients a predictable plan for both initial definitive treatment, as well as injection treatment of new cysts that fill up over time from the “solid” membranes that may be present. Microcystic injection therapy developed at Nationwide Children’s Hospital now offers patients a long-term option for percutaneous, minimally invasive treatment of new lymphatic malformation microcysts that are detected before they become problematic or develop into painful macrocysts.
Treatment options for lymphatic malformation include:
- Surgical removal
- Interventional radiology minimally-invasive ablation
- Medical therapy (not curative), along with sclerotherapy procedures
As a world center of excellence in radiology, the interventional radiology team at Nationwide Children’s Hospital has pioneered numerous minimally-invasive treatments for macrocystic, microcystic and solid lymphatic malformation in children and adults over the past two decades. Patients travel from around the world to Nationwide Children's Hospital for minimally-invasive treatment of lymphatic malformation.
While orbital lymphatic malformation is a unique challenge, our team provides the most comprehensive treatment solutions for outpatient treatment of both macrocystic and microcystic orbital lymphatic malformations. Patients have access to a full, multidisciplinary management team that includes oculoplastic and ophthalmologic surgeons, who have decades of treatment experience of orbital lymphatic malformations and vascular anomalies.
Transition of Care
Dr. Shiels dedicated his life to advancing the field of radiology in order to provide the best care to children in our community, across the country and around the world. As we remember and celebrate his work, we will remain ever-grateful for his passionate mentorship of our radiology team and staff – some of whom have worked side by side with Dr. Shiels for more than a decade. Everything Dr. Shiels learned over his career, he taught to and instilled in his staff including his revolutionary advancements in interventional radiology and ultrasound; treating lymphatic malformations; bone tumor ablation, aneurysmal bone cyst and salivary gland ablation. His passion inspires the entire team to continue delivering the best possible care to children everywhere and his legacy will live in the advancements we continue to make here at Nationwide Children’s.
Nationwide Children's Hospital Uses Two Main Lymphatic Malformation Treatment Techniques for Each:
Macrocysts (large cysts)
Macrocysts are treated by placing a drainage tube in the cyst through a small skin opening, draining the cyst fluid, and placing two drugs in the cyst to kill the cyst.
- The first drug is a medical detergent that “cleans” the cell covering, opening pores in the cell membrane.
- The second drug is ethanol (alcohol) that penetrates through the open pores, entering the cell to kill the cells within 15 minutes.
The drainage tube is left in place for 3 days while the injured cyst “oozes” fluid that is carried out by the drain for two days. On the third day, the injured area begins to heal with tissue “glue” that seals the treated area during the healing process.
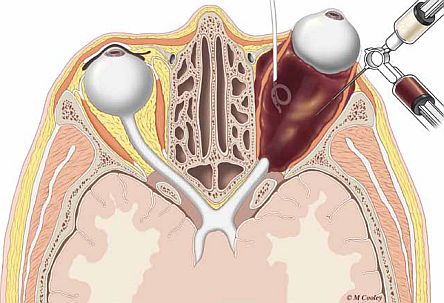
Above: this illustration demonstrates the use of a pigtail catheter to drain a cyst and the injection of solution to ablate the macrocyst. It also demonstrates the dual syringe method for aspirating and injecting doxycycline foam into lymphatic malformation microcysts.
Microcysts (small cysts)
Microcysts are treated and ablated with precise injection of a drug known as doxycycline. Injection of doxycycline into the microcysts is performed with a very small needle. The doxycycline is injected as a drug foam that looks and acts like meringue, similar to the topping of a lemon meringue pie. The body cleans up the killed lymphatic malformation from within, and heals the treated area without needing surgery to remove the dead tissue.
Above: this animation video shows the treatment of microcystic lymphatic malformation in the eye.
What happens if a lymphatic malformation is left untreated?
If a lymphatic malformation is left untreated, the large and small cysts can rapidly enlarge with bleeding and pain, or become infected. In areas such as the orbit, lymphatic malformation left untreated may result in severe pain, headaches and blindness.
What is sclerotherapy?
Sclerotherapy is injection drug therapy of a lymphatic malformation that kills the cyst within the body, without surgical scars or hospitalization.
How is sclerotherapy performed?
Macrocysts are treated by precisely placing a drainage tube in the cyst(s), most often with ultrasound camera guidance, through a small skin opening. With the tube in proper position, the cyst fluid is drained, cells obtained for microscopic diagnosis, and a radiology contrast agent (X-ray dye) is injected to fully define the cysts.
Treatment then begins by injecting two drugs in the cyst(s) to kill them. The first drug is a medical detergent that "cleans" the cell covering, which opens pores in the cell membrane. The second drug is ethanol that penetrates through the open pores, entering the cell to kill it within 15 minutes. The drainage tube is left in place for 3 days while the injured cyst "oozes" fluid that is carried out by the drain for two days. On the third day, the injured area begins to heal with tissue "glue" that seals the treated area during the healing process.
Microcysts are treated and ablated with precise needle injection of a drug known as doxycycline (an antibiotic that was found to kill lymphatic malformations as well as treat infections). Injection of doxycycline into the microcysts (each cyst individually injected) is performed with a very small needle, like the one used for a vaccine injection (example: tetanus shot). With ultrasound guidance, the needle is precisely placed into each microcyst, the cyst fluid drained, and doxycycline is injected as a drug foam. Developed at Nationwide Children’s Hospital, the foam looks and acts like meringue, similar to the topping of a lemon meringue pie. The doxycycline foam allows the interventional radiologists to precisely treat tens, or even hundreds, of cysts knowing which cysts have been treated and which remain to be treated. The body cleans up the killed lymphatic malformation from within and heals the treated area without needing surgery to remove the dead tissue.
Will my child be awake during the procedure?
Since the treatment involves placing needles precisely into the lymphatic malformation, most patients are treated while asleep with anesthesia.
How long will the procedure take?
Most treatments are performed within 1-2 hours, most often as outpatients without the need for hospitalization.
Are there any procedure risks?
Treatment risks are rare but may include infection, mild pain and mild swelling. Bleeding is usually not a problem and injury to tissues or organs next to the lymphatic malformation is avoided by precise placement of drainage tubes and injection needles.
What happens after the procedure?
Patients being treated for macrocystic and microcystic lymphatic malformation are discharged to go home (or to a hotel or the Ronald McDonald House). Patients who have macrocystic treatment are able to leave after they're awake following the treatment. They will have their drainage tubes in place during the 3-day drainage period. Patients who have microcystic treatment are able to leave following their treatment session. Patients most often have little or no pain or "recovery time" following the procedure.
When can my child bathe?
Patients being treated for macrocystic lymphatic malformation are not permitted to take baths or showers during the 3-day drainage period. Following drainage tube removal, patients are able to shower but should refrain from a submersion bath for 5 days after the drainage tube has been removed. Patients treated for microcystic lymphatic malformation are able to bathe and shower immediately following treatment.
Are there any activity restrictions?
Patients being treated for macrocystic lymphatic malformation can resume normal activities, avoiding activities that may cause the drainage tubes to be pulled or accidentally removed during the 3-day drainage period. Following drainage tube removal, patients are able to resume normal activities. Patients treated for microcystic lymphatic malformation are able to resume normal activity immediately following treatment.
Will the lymphatic malformation come back after the procedure?
Macrocystic and microcystic lymphatic malformation treatment is effective greater than 95 percent of the time, with the majority (85 percent) of macrocystic lymphatic malformation patients responding in a single treatment. Patients will be monitored annually for at least 5 years with ultrasound or MRI, watching for signs of new microcysts developing from solid lymphatic malformation tissue that is within the body. If and when new microcysts develop over time, minimally-invasive microcystic injection therapy can be planned before microcysts develop into painful macrocysts.
Will my child be in pain?
Macrocystic treatment is painless, with no cases of permanent nerve injury, muscle injury or other major complications. During the three days of catheter macrocyst drainage (after treatment), most patients (including orbit lymphatic malformation) are fully mobile and functional, without pain. Patients undergoing microcystic treatment may experience mild pain for two to four hours, responsive to oral narcotic analgesic therapy.
What can my child expect after treatment is complete? Any long-term effects?
Following treatment, patients are able to resume normal life activities, including sports. Patients undergo annual follow-up ultrasound or MRI examination (minimum five years) to evaluate for new microcysts that may mature from remaining solid LM tissue. New microcysts, if any, that develop are readily treated with simple microcystic needle injection therapy as an outpatient. In the past 15 years, greater than 95 percent of patients respond with complete success of macrocystic and microcystic lymphatic malformation components.
Patients treated at Nationwide Children’s Hospital from states other than Ohio (or other countries) undergo clinical follow-up with their local referring physicians and send imaging studies for Nationwide Children’s radiologists to review, for telephone follow-up and future treatment decision-making.
Our Patient Outcomes
Patients who have undergone treatment for lymphatic malformation at Nationwide Children’s Hospital, range in age from 1 month to 60 years. Locations of percutaneous treatment for lymphatic malformation include the orbit, ear, neck, head, arm, leg, hand, foot, axilla, mediastinum, chest wall, abdomen, scrotum and penis. Most procedures are performed as definitive first-line therapy, with occasional patients referred after surgical debulking or following surgical recurrence. Procedures are performed in the interventional radiology suite under deep, intravenous anesthesia or general anesthesia. Treatment is divided into two therapeutic regimens, one for macrocystic disease and one for microcystic disease. Most lymphatic malformation treatments are performed as outpatients, with extensive cases involving a one-night stay in the hospital for intravenous antibiotic therapy and fluid management.
In the treatment of large cysts, there is a 15% incidence of repeat hemorrhage in macrocysts following initial sclerotherapy. Following repeat hemorrhage, a second treatment has been effective for ablation in 100% of cases, without scarring or functional limitation. In our patients, no cases of neuropathy, unexpected skin necrosis or myoglobinuria have been encountered with sclerotherapy. Microcystic lymphatic malformations are successfully treated with 1-3 treatments in greater than 95% of patients.



