Spina Bifida and Myelomeningocele
Spina bifida (Latin for “split spine”) is a type of neural tube defect, which is a problem with the spinal cord or the structures that cover it.
What Is Spina Bifida?
Spina bifida is a congenital (happening before birth) condition where a part of the baby’s spinal cord develops outside instead of inside the bones of the spine. There are different types of spina bifida, including myelomeningocele, myeloschisis, meningocele, and spina bifida occulta. Spina bifida is a rare condition that can happen anywhere along the spine. It often happens in the lower back.
What Causes Spina Bifida?
No one knows the exact cause of spina bifida. Not getting enough folic acid during pregnancy may be a risk factor.
How Is Spina Bifida Diagnosed?
Most diagnoses of spina bifida are made during pregnancy with a non-invasive test that takes pictures of the baby, called an ultrasound. This is done by looking at the shape of the brain. Spina bifida is often diagnosed when the brain develops in the shape of fruit, like lemons or bananas. These are called fruit signs. The ultrasound can also show where the opening is in the spine, problems with your baby’s legs, and early signs of fluid buildup in the brain.
The following tests may be used to diagnose spina bifida:
- Anatomy ultrasound – a high-resolution ultrasound to confirm the diagnosis and check for other problems.
- Fetal MRI – non-invasive imaging that gives more details of the baby’s organs that may not be seen on an ultrasound.
- Fetal echocardiogram – a special ultrasound to check the baby’s heart structure and function.
- Blood work – This is a blood test that can show if there are high levels of alpha-fetoprotein (AFP) in the pregnant patient’s blood. If the levels are high, doctors may suspect spina bifida.
Genetic Tests
For a small number of babies with spina bifida, there may be other genetic conditions. Genetic testing can help doctors decide if your baby will need surgery before they’re born. This is called fetal surgery. Some genetic tests include:
- Cell-Free Fetal DNA Testing: A sample of blood is taken to look for copies of your baby's DNA. A positive result means there could be problems with the DNA. Another test must be done to confirm the results. Other testing may be done before or after birth, depending on your baby’s needs.
- Amniocentesis: A small sample of amniotic fluid that surrounds the baby in the womb is taken and tested for DNA problems. This test is usually done in the middle of the second trimester of pregnancy, usually between 15 and 20 weeks. It can be used to confirm findings from the cell-free fetal DNA test.
- Karyotype or Microarray: These tests can be done before your baby is born through an amniotic fluid or placenta sample. They can also be done after the after birth through blood sample from the umbilical cord. They both check for DNA problems. A karyotype is a basic chromosome study and a microarray is a more detailed look at all genes.
Types of Spina Bifida
Myelomeningocele. This is the most common type of spina bifida. It can be very serious since the spinal cord is exposed through the skin through a thin-walled sac. This makes it easier to damage and keeps it from working the right way.
This condition can affect:
- The nerves that control your baby’s hips, thighs, and leg muscles. This can affect how your baby moves. They may have problems with the bones as well due to weak muscles in the back and legs. These include a curved spine (scoliosis) and dislocated hips, bones, joints, or feet.
- The cerebrospinal fluid (CSF) in the brain. CSF can leak and build up in the brain, creating pressure. This is called ventriculomegaly. Children with this condition may have a tube, called a shunt, placed after they are born to drain the extra fluid.
- The bladder and bowel. This condition may affect your child’s ability to control their own pee and poop (stool). There are many urinary and bowel programs that can help your child have better control with these.
Surgery is needed within 1 to 3 days after birth to close the opening. It cannot fix the damage that has already occurred to the nerves. It can help prevent further damage and reduce the chance of infection.
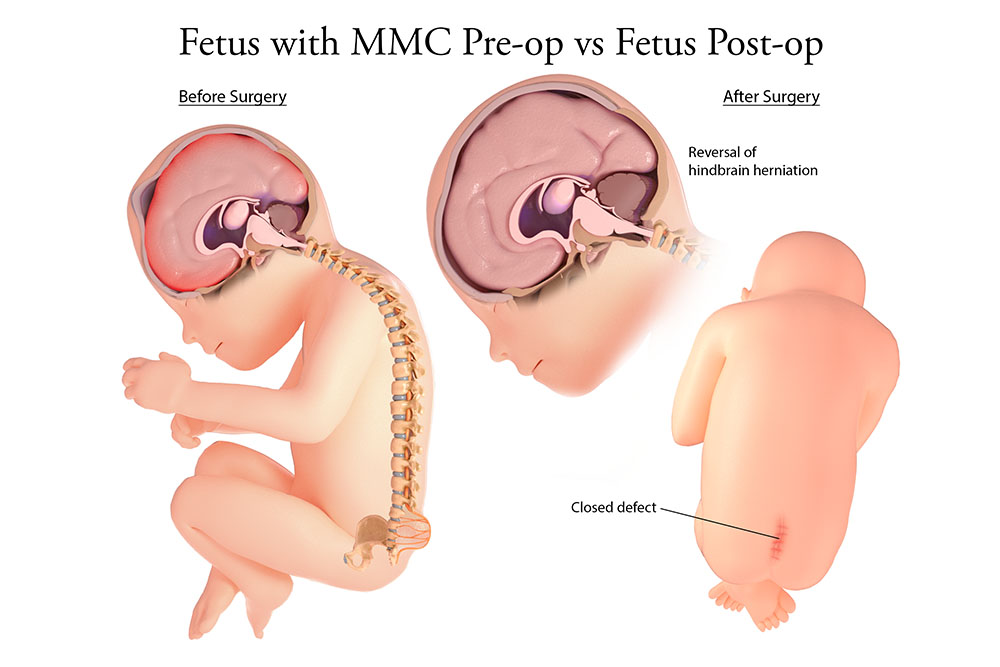
Closure of the myelomeningocele can result in reversed hindbrain herniation.
Myeloschisis. This is a serious condition where the spinal cord and surrounding nerve tissue are exposed to amniotic fluid. Myeloschisis has a flat neural tube without a layer of skin covering the opening in the spine. Myeloschisis symptoms are like those of myelomeningocele.
Meningocele. This is a less serious form of spina bifida. A sac of fluid comes through the baby’s back and can be seen outside as a lump or bulge along the spine. The spinal cord and nerves are not in the sac. This type of spina bifida can cause some problems. The timing of the surgery to close the meningocele is decided by your child’s neurosurgeon.
Spina bifida occulta. This is the mildest form of spina bifida. The bones in the lower back around the spinal cord and nerves don’t form the right way. The baby may have a hairy patch, dimple, or birthmark over this opening, but there is no opening or sac. In this condition, the nerves at the end of the spinal cord may not work the right way. This is called a tethered spinal cord. This type of spina bifida is not usually found when you’re pregnant.
Other Problems That Can Happen With Spina Bifida
Some other conditions that children with spina bifida may have include:
- Hydrocephalus – A condition where the fluid inside and around the brain builds up. This causes pressure on the brain or spinal cord. Surgery may be needed to relieve the pressure.
- Chiari II malformation – A condition where a part of the brainstem and the lower back part of the brain (called the cerebellum) are pulled down through the base of the skull. The cerebellum controls coordination and balance, and the brainstem controls functions, like breathing, heart rate, and swallowing. Chiari II can cause hydrocephalus and other problems. Surgery may be needed to relieve the pressure on the brain.
- Neurogenic bladder – A condition where the nerves in the spinal cord that control the bladder do not form correctly. This means that your child’s bladder will have trouble holding pee, emptying the bladder (peeing), or both. They may need a catheter to remove pee and help them keep as much kidney and bladder function as possible.
- Neurogenic bowel – A condition where the nerves in the large intestine (bowel) do not form correctly. This can cause problems storing poop (stool), emptying the poop, or both. Your child may be constipated and need treatment.
- Leg weakness and decreased feeling – This condition may include not being able to move parts or most of the lower limbs (paralysis). Some children may be able to walk using braces, crutches, or walkers. Some may need a wheelchair later in life.
- Clubfoot – This is a condition where the bones of the foot and lower leg do not develop normally. The foot turns in and down and stays tight in this position. This can happen with severe leg weakness or paralysis, common in myelomeningocele.
- Learning problems –These can be different for each child but may include issues with problem solving, memory, self-control, paying attention, language, reading, and math.
Care During Pregnancy
If you are carrying a baby with spina bifida, you will keep getting care from your obstetrician (OB/GYN). They may refer you to The Fetal Center at Nationwide Children’s Hospital. There, you will work with a team that includes:
- Maternal-Fetal medicine doctor
- Neonatologists: Doctors who take care of newborns
- Neurosurgeons: Doctors who do surgery on the brain and spinal cord
- Urologists: Doctors that take care of problems with the kidneys and bladder
- Geneticists and genetic counselors: Experts in medical genetics and counseling
- Nurses: Help care for your baby and teach you how to care for your baby
- Nurse coordinators: Guide you through your pregnancy and prepare you for what to expect
How Is Spina Bifida Treated?
Treatment During Pregnancy
Your child may need fetal surgery to protect the exposed spinal cord from injury, improve function, and decrease problems later in life. However, any nerve damage that has taken place before surgery can’t be fixed. If fetal surgery is not an option for you and your baby, the exposed spinal cord is closed by surgery soon after birth. Your child will have a team of experts to give them early treatment for any problems.
Your Fetal Center health care team will talk to you about the prenatal test results and the treatment plan that’s best for you and your baby.
In some special cases, fetal surgery can greatly reduce the need for a shunt after birth and improve the chances of walking. It does, however, increase the risk of delivering your baby early and other maternal problems. Fetal surgery is usually done between 22 and 25 weeks. How the surgery is done will be based on the ultrasound and MRI findings.
You will need to meet with the Fetal Center medical team to make sure fetal surgery is an option for you and your baby. This includes members from neonatology, neurosurgery, nursing, and social work. At the appointment, you will have a:
- Fetal MRI (magnetic resonance imaging)
- Fetal echocardiogram
- Details fetal ultrasound
- Amniocentesis
Types of Fetal Surgery for Spina Bifida
- Open Fetal Surgery – During open fetal surgery, the surgeon makes a cut (incision) right below the pregnant patient’s belly button and into the uterus. During this surgery, the mother must be under general anesthesia. Medicines will be used before, during, and after the surgery to help control pain and relax the uterus to prevent contractions. The placenta will still get oxygen and nutrients during surgery. The anesthesia passes through the placenta to control pain for your baby. In some cases, the baby is also given medicines to help with pain. During surgery, the spinal cord is returned to the correct spot, and the layers of protection and skin around the spinal cord are closed. The mother’s uterus and abdomen are then sewn back together. These surgeries can be done through a very small cut (less than 2 inches) in the uterus. This is called a mini-hysterotomy and helps reduce problems with the pregnancy.
After any open fetal surgery, the mother must deliver by cesarean section (C-section) around 37 weeks. This prevents any stretching or tearing of the scar on the uterus from the fetal surgery.
- Fetoscopic procedure – This procedure uses smaller cuts (incisions) than open surgery. Anesthesia is given through a shot in the pregnant patient’s spinal cord. This is called an epidural. General anesthesia may be used if it’s needed. During this procedure, tiny cameras and surgery tools are put into the small incisions to operate on the baby. During surgery, the spinal cord is returned to the correct spot, and the layers of protection and skin around the spinal cord are closed. The small cuts on the womb are sewn back together. This surgery may take longer than open surgery, but it has less risks.
- Vaginal delivery after a fetoscopic procedure may be possible if there are no other problems with the pregnancy.
Risks of Fetal Surgery
The main risks of fetal surgery includes:
- Early delivery
- Early breaking of the amniotic sac (premature rupture of membranes)
- Problems with the healing of the uterine scar
- Infection (rare)
- Bleeding (rare)
- Problems with anesthesia (rare)
Care After You Baby Is Born
At the delivery hospital, your baby will be cared for in the neonatal intensive care unit (NICU). A doctor who specializes in treating newborns (neonatologist) will manage their care.
Right after delivery, your baby will:
- Get an intravenous (IV) line in their arm, hand, foot, or head. The IV gives fluids, medicines, nutrients, and antibiotics to prevent dehydration and infection.
- Go to the main Nationwide Children’s Hospital NICU for the rest of their care.
Surgery After Birth (Postnatal Surgery)
- The surgery to repair myelomeningocele is needed within 24 to 72 hours after your baby is born in babies that didn’t have fetal surgery.
- Surgery for hydrocephalus will be done after birth by placing a hollow tube (shunt) to drain the extra fluid, if needed. The timing of the surgery depends on your baby’s symptoms and condition. The medical team will talk to you about the best time for surgery. Babies that had fetal surgery lower the chance of needing this surgery by half.
Care After Surgery
After surgery, your baby will be cared for in the NICU. How long they are there depends on any other issues they may have. Their care will involve appointments (consults) with many different doctors and medical specialists and include other tests and procedures.
Some of these may include:
- Brain imaging test: This could be an ultrasound or MRI of the brain to check for hydrocephalus and Chiari II malformation.
- Urology consult – This looks at your baby’s kidneys and bladder. They will need a small tube inserted into the urethra to empty the bladder and let pee out. This is called catheterization. Parents will learn how to do this at home.
- VCUG and renal ultrasound: These are imaging studies that can give doctors information about how the bladder and kidneys are working.
- Orthopedic consult: A specialist will check for spine, hip, leg, and clubfoot problems.
- Physical medicine consult: A doctor will diagnose and treat problems related to the nerves, muscles, bones, and brain that could cause short-term or long-term problems.
- Genetics consult: A geneticist will work with you and discuss the risk of having another child with this condition.
- Developmental pediatrics and myelomeningocele consult: These specialists will see your baby in the NICU and follow them until it is time to leave the hospital. They can help with care plans and discharge needs.
- Physical and occupational therapy evaluation: These therapists will assess your baby and provide early intervention and therapy so they can function as best as possible.
Feedings
Your baby will start with small amounts of human milk or formula. The amount will be increased slowly. When your baby is taking enough milk or formula to grow and gain weight, their IV will be removed.
Discharge Planning:
We will teach you to care for your baby at home. We will show you how to:
- Take care of skin to keep it healthy and keep it from breaking down.
- Learn how to catheterize your baby.
- Feed your baby.
- Help your baby move.
- Interact with your baby.
Looking Ahead
Spina bifida is a lifelong condition that can’t be cured. The goal of care is to prevent problems and keep your child as healthy as possible. They will need regular appointments with a local pediatrician or health care provider to measure growth, development, nutrition, and immunizations. The program coordinator can help you find one if needed. Your baby will have follow-up appointments with pediatric neurosurgery and the myelomeningocele clinic for care related to spina bifida.
With help, children with spina bifida do well in school, play sports, and live full lives into adulthood. Each child will face different challenges and need different treatments. This is important, as more may be understood about your child’s condition as they grow.
Future Pregnancies
Your doctor may recommend genetic counseling to find out the risk of spina bifida for a future pregnancy. Women who have a child with spina bifida should take 400 mcg (4 mg) of folic acid each day for 1 to 3 months before getting pregnant. They should keep taking it during the first 3 months of pregnancy. Taking folic acid does not mean your baby will not have spina bifida, but it will reduce the risk.



