NICU Follow-Up Programs
Your Baby’s Development Matters To You: And It Matters To Us.
NICU Follow-up Programs
We know that you are the most important person in your NICU graduate’s life, and that you will have the greatest impact on your baby’s development. The NICU Follow-up Program cares about how you and your baby grow together.
After going home from the NICU, your baby is at high risk for medical and developmental problems and we believe that he/she deserves the best possible follow-up program. When we identify medical and developmental needs as early as possible, we can provide the services and family support needed to make a lasting difference. We also support the medical needs of babies who have conditions such as bronchopulmonary dysplasia (BPD) or neonatal abstinence syndrome (NAS).
Our team includes medical and developmental specialists who work with your pediatrician and other community providers. We carefully evaluate your baby and family’s needs at regular intervals in the first three years using the newest and best tools available.
Together, we can make the journey toward your child’s best outcome.
Now Offering Telehealth Appointments
Learn more about our telehealth services at Nationwide Children's.
Your NICU Follow-Up Programs Team
We are an interdisciplinary team that addresses the medical, nutritional, neurological, developmental and social needs of patients in a single location.
Our staff has extensive experience in caring for high-risk and premature infants.
Our neonatal team includes:
- Neonatologist
- Pediatrician
- Psychologists
- Pediatric Neurologist
- Certified Pediatric Nurse Practitioner
- Physical Therapists (PT)
- Occupational Therapists (OT)
- Speech Language Pathologist
- Nurse Clinician
- Social Worker
- Registered Dietitian
- Lactation Consultant
Our Clinics
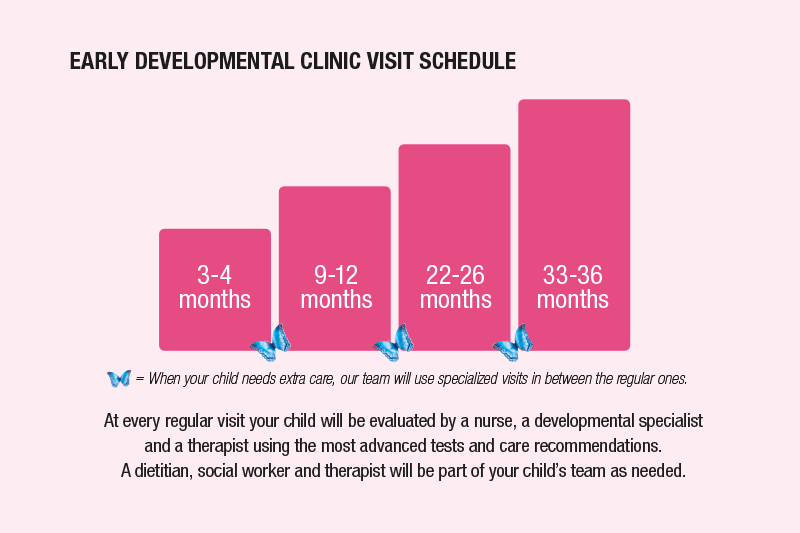
Early Developmental Clinic
Our clinic cares for babies born early or with challenges at birth at risk for delays in growth and development. We offer the best and newest tests to identify and diagnose problems in the early years of development. We support babies and families with specialized services, immediate referrals, and continuing education, and provide care to toddlers with complex problems such as cerebral palsy and behavioral disorders until age 3. We also follow babies who began care in one of the other specialized clinic programs.

BPD Clinic
We specialize in babies diagnosed with moderate to severe bronchopulmonary dysplasia (BPD) who need oxygen when going home. We partner with your pediatrician to help coordinate care and provide specialized services. We offer comprehensive care by a team of medical provider, dietician, nurse, and social worker, with all care and medication management tailored to help you support healthy grown and development of your child. All babies seen in BPD clinic are followed in the Early Developmental Clinic until age 3.
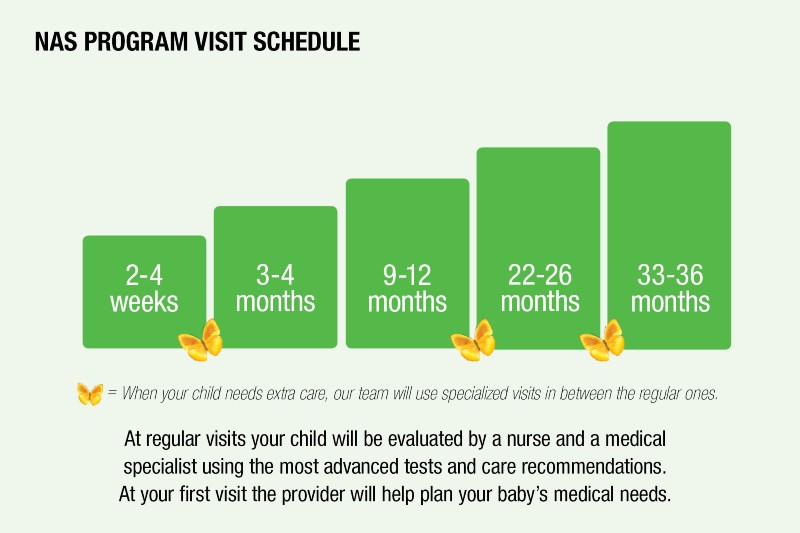
NAS Program
We see babies who had certain exposures during pregnancy or after birth because they are at risk of developing medical symptoms when they go home or developmental delays. If necessary, we help wean your baby off medications and make sure your baby is doing well off of these. Your pediatrician can refer your baby to our clinic any time before age 3, if needed. All babies seen in the NAS program are followed in the Early Developmental Clinic until age 3.
Giggle ‘n Groove Music Therapy Classes
We offer research-based music therapy classes every Wednesday in the community to aid your baby’s growth and development through music and play activities. Giggle ‘n Groove classes are offered at our Westerville and East Columbus Close-to-Home centers, for infants and toddlers 6-24 months. You can find the right age group and time that works for your child below!
Research
Hearing, Speech and Sound
Our team is composed of a large group of physicians and therapists focused on Hearing, Speech and Sound Environment. We use brain-based measures to investigate mechanisms of cortical and subcortical hearing development. We study both typical children and those at high risk of delays and hearing impairment. We characterize their response to various environmental conditions and sound-based interventions. Ultimately, we are most interested in the effect of hearing development on language and communication. We also study the relationship between early neurophysiology and later development of communication skills. Many of our publications and studies investigate assessment tools and interventions in this field.
Sensory and Motor
The sensory environment in the NICU may have dramatic and lasting effects on perceptual, cognitive, and emotional development of preterm infants. In babies, supportive experiences (skin-to-skin care, breast feeding) are associated with stronger brain responses than painful experiences. Babies born premature also have reduced response to touch. We recognize the importance of parent involvement in outcomes of their child. We are conducting a randomized trial to determine whether a multisensory intervention combining gentle touch with mother’s voice (see MIND study) improves the neurodevelopmental outcomes in preterm infants. We are also conducting a randomized trial using a parent-administered intervention to improve sensorimotor outcomes for children with neurodevelopmental disorders (see APPLES study).
Parenting & Emotional Connection
Engagement between mothers and infants activates specific responses in their brains. We are comparing the neural responses of infants who have suffered a brain insult or injury compared to responses in typical mother infant dyads. Both mother and infant wear special EEG caps to non-invasively measure brain responses to interactions between mother and infant (e.g., looking, smiling, speaking). This approach reveals how infants’ brains process the mother’s infant-directed sensory input, which is necessary in these pre-verbal subjects. Knowledge gained may help to design new parent-based developmental interventions for use in the NICU and in the early developmental period.
We are also examining the role that parenting style plays in neural development of infants. In combination with techniques to measure how infant brains respond to infant-directed speech, we are examining the role of parenting style affects the emotional connection within the mother infant dyad. The goal is to develop high quality interventions to modify parenting approaches to improve infant outcomes.
International Activities
The BBOP Team has many national and international collaborations. For example, we are involved in the REACH (Rehabilitation very EArly in Congenital Hemiplegia) multisite randomized trial coordinated by researchers in Australia that is comparing parent-led modified constraint-induced movement therapy (CIMT) to bimanual therapy (BIM) in infants (3-9 months) with upper extremity asymmetries. Team members also conduct workshops to train therapists on administration of the Hammersmith Infant Neurological Exam, one of the recommended tools to screen infants at high-risk for cerebral palsy and other neurodevelopmental disorders.
Optimal Use of an FDA-Approved Device for PDA Closure in Infants
Our team is providing the neurodevelopmental follow-up for infants participating in this large study. Click hear to read the article in Pediatrics Nationwide.
Scheduling an Appointment
- We will help you set up your baby’s appointment before you go home from the hospital. Your baby’s NICU case manager will schedule a convenient appointment for you.
- If you and your baby received NICU care at a different hospital, we can also help. Please call us to set up your appointment at (614) 722-4530.
- If you have concerns about transportation to the clinic, let the case manager and the clinic staff know. We want to help you and your baby make it to this very important visit.
- You will receive a confirmation call and confirmation letter for your appointment. You also have the option to choose a text reminder.
