Atrial Septoplasty

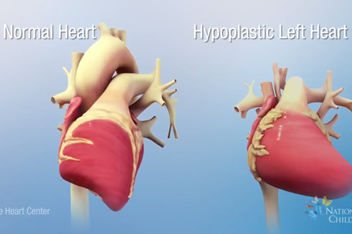
What is Hypoplastic Left Heart Syndrome with an Intact / Restrictive Atrial Septum?
In some unborn babies (fetuses) with hypoplastic left heart syndrome (HLHS), there is either no hole or too small of a hole in the wall between the top chambers of the heart. This problem is called an intact or highly restrictive atrial septum. The atrial septum is the wall between the top two chambers of the heart. When there is no hole, the blood returning from the lungs into the left upper chamber cannot move to the rest of the body. This is because the left side of the heart did not grow, and the hole is too small or not there at all. This makes blood back up in the lungs, causing lung damage. The chance of early death after delivery is much higher (about 50% risk of death) than in a fetus with HLHS who has a normal hole in the atrial septum. Those babies only have about a 15% risk of death before going home. Advances in technology have helped to diagnose intact or restrictive atrial septum in infants before birth. This problem can be found by a fetal echocardiogram as early as 18 weeks into the pregnancy. In some fetuses, there may be a chance to fix this problem by opening up a hole in the atrial septum before birth. Opening the atrial septum will not keep the fetus from getting HLHS but may lower the risk of lung damage.
Procedure: Atrial Septal Balloon Dilation or Stent
First, the mother has an epidural placed. An epidural is a small, flexible, hollow tube that is placed into the mother’s lower back. This tube gives the mother pain (anesthesia) medicines that have little to no effect on the fetus. A needle is used to provide pain medicine to the fetus through an injection in the thigh of the fetus. Next, a needle is inserted into the mother’s abdomen and uterus and into the fetal heart (Picture 1). The doctor will use ultrasound guidance to do this. Radiation is not used for the procedure.
A wire and balloon are placed through the needle and across the atrial septum (Picture 2). A balloon or a balloon with a wire tube (stent) (Picture 3) is inflated in the atrial septum to make a larger or a new hole between the chambers.
After the procedure, doctors watch the mother and baby with many fetal ultrasounds and fetal echocardiograms to find and treat any concerns so that the mother may carry the baby as close to full-term as possible. This gives the lungs, brain, and other vital organs a chance to grow as much as possible before birth.
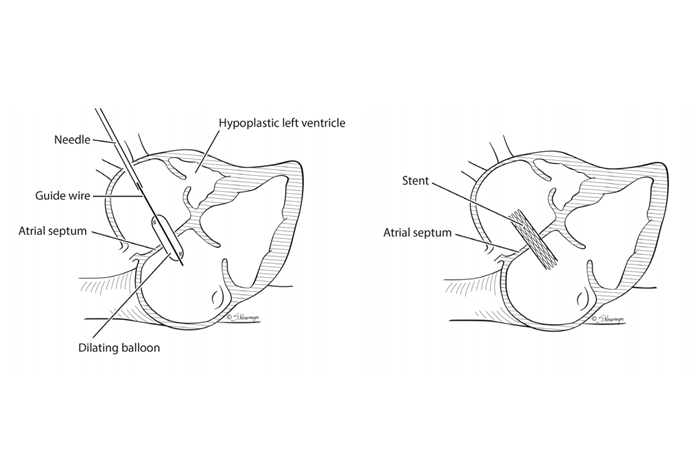
Picture 2 (left): Fetal atrial septal balloon dilation
Picture 3 (right): Fetal atrial stent dilation
Benefits of the Procedure
The goal of surgery on the baby while still in the womb (in utero) is to open the blocked atrial septum with a balloon and/or stent before damage is done to the fetus’s lungs. Opening the blocked septum and restoring normal blood flow can decrease pressure in the left atrium, giving the lungs time to heal before birth. The goal of the procedure is to give the fetus better blood flow to the lungs, lowering the chance of needing emergency surgery right after birth. The ultimate goal is to improve the chances of survival for the baby, but this is still unknown about this surgery.
Other Options
There are no other procedures or alternative intervention to fix this problem in utero. However, not doing the procedure is an option. The emergency procedure could be tried right after delivery though the potential for improvements in lung function is less than if the procedure is done before birth.
Even with the best medicines and surgery, only 50% of babies with HLHS with intact atrial septum survive to go home after birth.
Risks of the Procedure
Risks to the Mother
The mother is at risk for problems due to anesthesia. These problems could be nausea/vomiting, spinal headache, bleeding (in utero or vaginal), infection, leakage of amniotic fluid, and preterm labor or delivery. The procedure is done under sterile ultrasound guidance, and medicines are given to calm the uterus and lower these risks.
Risk to the Fetus
If a stent is used in the procedure, there is a risk of the stent moving out of position after the stent is placed. The fetus is at risk for developing a blood collection around the heart (hemopericardium). Hemopericardium can be treated by removing the blood with a needle like the one used for the procedure. There is risk of damaging other parts of the heart close to the sac during this procedure. The fetus is also at risk for having a heartbeat that is too slow (bradycardia). Before the procedure, the fetus is given medicine to lower the risk of getting bradycardia. There is a 10% risk of preterm labor
or delivery and 10% risk of loss of the fetus.