Aortic Stenosis Balloon Valvuloplasty

What is Critical Aortic Stenosis?
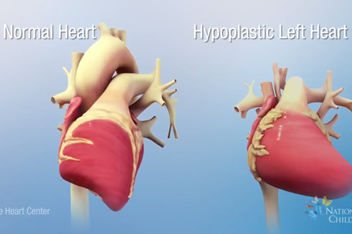
In the normal fetal heart, blood flows from the heart through the aortic valve to the rest of the body. The term ‘aortic stenosis’ means narrowing of the aortic valve. Critical means the narrowing is severe. This limits blood flow to the body. This may be the only heart problem your child has or there may be other problems. Aortic stenosis may be seen with a fetal echocardiogram as early as 16 weeks into the pregnancy. When critical aortic stenosis is present in a second-trimester fetus, the left ventricle, or pumping chamber, becomes enlarged and weak. As a result, there is less blood flow through the left heart. This causes the left ventricle to stop growing, making the left heart too small. This condition is called hypoplastic left heart syndrome (HLHS). Instead of the normal two pumping chamber heart, patients with HLHS have one pumping chamber. This one chamber must send blood to both the lungs and body all on its own. This causes both short- and long-term problems for these children, including many open heart surgeries, catheterization procedures, and, eventually, heart transplantation. In some patients, there is a chance to reverse this problem by opening up the aortic valve in the fetus.
Procedure: Fetal Aortic Valve Balloon Dilation
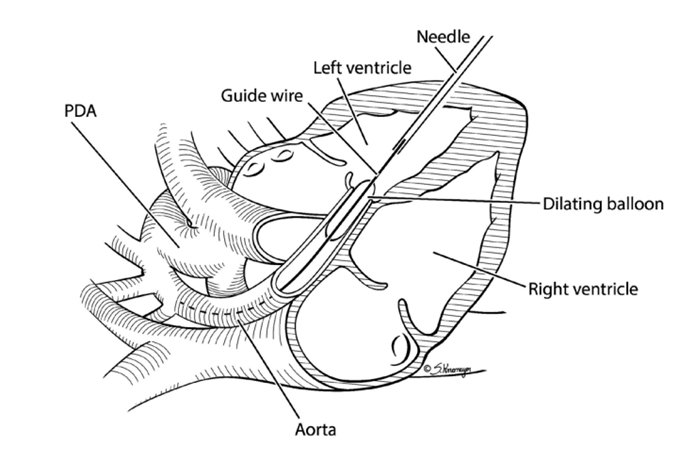
First, the mother has an epidural placed. An epidural is a small, flexible, hollow tube that is placed into the mother’s lower back. This tube gives the mother pain (anesthesia) medicines that have little to no effect on the fetus. A needle is used to provide pain medicine to the fetus through an injection in the thigh of the fetus. Next, a needle is inserted into the mother’s abdomen and uterus and into the fetal heart (Picture 1). The doctor will use ultrasound guidance to do this. Radiation is not used for the procedure.
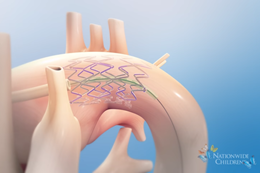
A wire and balloon are placed through the needle and across the aortic valve. The balloon is then gently inflated to make the opening of the aortic valve bigger (Picture 2).
After the procedure, doctors watch the mother and baby closely with many fetal ultrasounds and fetal echocardiograms to find and treat any concerns so that so that the mother may carry the baby as close to full-term as possible. This gives the lungs, brain, and other vital organs a chance to grow as much as possible before birth.
Benefits of the Procedure
The goal of surgery on the baby while still in the womb (in utero) is to open the narrowed (stenotic) aortic valve before the left ventricle can shrink or is forced to stop growing. Opening this valve may improve blood flow in and out of the left ventricle and allow it to keep growing during pregnancy. If normal blood flow can be restored, the baby may have a normal-sized, functioning left ventricle at birth.
Other Options
Visit our animation library to learn more about the Hybrid Stage 1, Hybrid Stage 2 and Fontan procedures for treating HLHS.
There are no other procedures or alternative interventions to fix this problem in utero. However, not doing the procedure is an option. For those babies that have HLHS, there is a series of three heart surgeries to re-route blood flow so that the right heart pumps blood to the body (normally the job of the left heart). Some children need more than three heart surgeries and multiple catheterizations.
Even with the best medicines and surgeries, only 75% of babies survive to one year of age.
Risks of the Procedure
Risks to the mother
The mother is at risk for problems due to anesthesia. These problems could be nausea/vomiting, spinal headache, bleeding (in utero or vaginal), infection, leakage of amniotic fluid, and preterm labor or delivery. The procedure is done under sterile ultrasound guidance, and medicines are given to calm the uterus and lower these risks.
Risks to the Fetus
The fetus is at risk for developing a blood collection around the heart (hemopericardium). Hemopericardium can be treated by removing the blood with a needle similar to the one used for the procedure. There is risk of damaging other parts of the heart close to the sac during this procedure. The fetus is also at risk for having a heartbeat that is too slow (bradycardia). Before the procedure, the fetus is given medicine to lower the risk of getting bradycardia. There is a 10% risk of preterm labor or delivery and 10% risk of loss of the fetus.