Diabetes: Insulin Dependent Diabetes Mellitus (Type I)
![]()
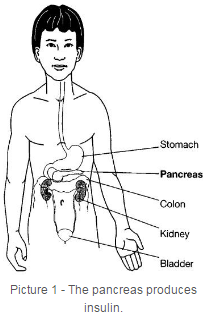
Insulin dependent diabetes mellitus (IDDM), also known as type 1 diabetes, usually starts before 15 years of age, but can occur in adults also. Diabetes involves the pancreas gland, which is located behind the stomach (Picture 1). The special cells (beta cells) of the pancreas produce a hormone called insulin.
The body is made up of millions of cells. All cells need glucose (sugar) from the food we eat for energy. Just as a car can’t run without gasoline, the body can’t work without glucose. Insulin is the “key” that allows glucose to enter the cells. Without this key, glucose stays in the bloodstream and the cells can’t use it for energy. Instead, the glucose builds up in the blood and spills over into the urine. When a person develops type 1 diabetes, the pancreas stops making insulin. To help the body’s cells use the glucose, a child with type 1 diabetes mellitus (DM) must receive insulin by injection (shot).
What Happens in Type 1 Diabetes
The cause of diabetes is not known. Some experts believe diabetes is inherited (runs in families), but the genetics are not clearly understood. Diabetes does not always run in families. The body mistakes the cells that produce insulin for foreign cells. The body then destroys these cells. This is called an auto-immune process. Although something in the environment may trigger the disease, there are no known ways to prevent type 1 diabetes in children.
Important Facts about Diabetes
People do not “outgrow” type 1 diabetes, but they can learn to control it by insulin shots, blood glucose testing, diet and exercise.
Diabetes is not contagious ("catching").
About 14.6 million Americans have diabetes.
About 1 out of 10 people with diabetes have type 1 DM.
Another type of diabetes is type 2, non-insulin dependent diabetes mellitus (NIDDM). Type 2 diabetes is more common than type 1. About 9 out of 10 people with diabetes have type 2. Type 2 DM used to occur mostly in adults, but is becoming increasingly more common in children. It is associated with obesity. NIDDM usually starts after 40 years of age. People with type 2 diabetes usually produce enough of their own insulin, but their bodies don’t use it right. Type 2 may be controlled by weight loss or with insulin and/or oral medicine.
Signs of Diabetes Mellitus
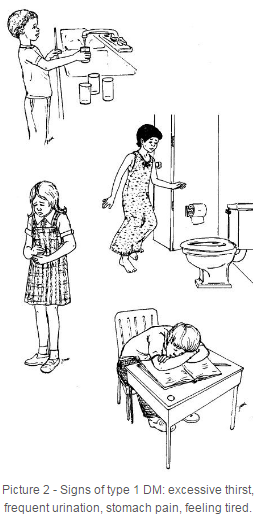
Type 1 usually comes on suddenly.
Early Signs of Type 1 DM Are (Picture 2):
- Weight loss or poor weight gain, even if eating large amounts of food
- More thirst than usual
- Enuresis (bed wetting)
- Frequent urination
- More urine than usual
- Feeling tired all the time
Later Signs of Diabetes Are:
- Dry skin and mouth
- Hard to breathe
- Urine sugar and acetone will be positive
- Blood sugar is very high (above 126 mg/dL)
- Loss of appetite
- "Fruity" odor to the breath
- Stomach pain
What Causes Glucose (Sugar) in the Urine
The kidneys filter waste products and excess water out of the blood. When the glucose in the blood is above normal level, the kidneys can’t hold it all. The glucose then shows up in the urine. The glucose in the urine causes the urine output to increase in frequency and amount. This increase causes you to be thirstier.
What Causes Acetone (Ketones) in the Urine
When the body can’t use glucose because of the lack of insulin, the body uses fat for energy. This causes weight loss. When large amounts of fat are broken down too quickly, acetones (ketones) are produced. Acetone builds up in the blood and "spills over" into the urine. Too many ketone acids in the blood may result in ketoacidosis. (Refer to the Helping Hand: Diabetes: Ketoacidosis, HH-I-23.)
The Honeymoon Period
Shortly after you find out you have diabetes and start treatment, your need for insulin may be a lot less. This is because the pancreas cells that make insulin have not yet been completely destroyed. They begin to make a small amount of insulin. We call this the “honeymoon period”. If a honeymoon period occurs, it starts shortly after diagnosis and can last anywhere from two weeks to two years. You will need to continue to take small amounts of insulin during this time. After the honeymoon period is over, the pancreas will no longer produce insulin and insulin needs to go up.
Treatment
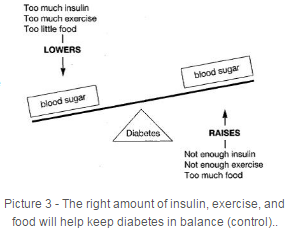
There must be a balance between insulin, food, and exercise to keep your diabetes under control (Picture 3). Education is necessary to help you and your family understand how to properly take care of you and your diabetes.
Insulin
Insulin is made in the laboratory using a chemical process. There are a number of types of insulin. Your doctor will prescribe the kind that is best for you. You will need multiple shots of insulin every day. It is given by injection. Your nurse will teach you and your parents how to give the insulin shots.
Meal Plan
You will need foods that help your body grow, produce energy and keep your blood sugar in balance. Your dietitian will help to set up a meal plan based on your age, gender, and activity level. Ask your diabetes nurse educator or dietitian about how you can learn to include all food groups how to count carbohydrates so you can have a flexible meal plan.
Your dietitian will teach you and your parents about meal planning.
Exercise
Exercise builds muscles, keeps the body in shape, improves general health, helps keep you mentally alert and increases the heart muscle tone. Exercise improves the way insulin is absorbed and used by the body. And it usually makes the blood sugar go down. Include exercise in your daily plan.
Monitoring
Monitoring your diabetes means checking to see if it is under control. It will help you and your parents know if the treatment plan is working well. We will teach you and your family how to measure blood sugar and urine ketones. Blood testing is one way to check to see if your diabetes is under control. Learn to use a logbook or fax log sheet to record your blood sugars. The doctor will tell the lab to do a blood test that measures your average glucose level over the last 3 months. This test is called glycosylated hemoglobin, or Hemoglobin A1-C, and is usually done every 3 to 4 months. Your nurse educator or doctor will tell you more about daily monitoring. Refer to the Helping Hand: Diabetes: Self-monitoring of Blood Glucose, HH-I-22. Hemoglobin A1-C less than 7% will help prevent complications from occurring.
Education
Education about diabetes, daily attention to meals, exercise, insulin and proper care of your body are all necessary to control your diabetes and continue with normal daily living. Your doctor, nurse, dietitian and other persons in the health care field will teach you all about diabetes.
If you have any questions, please be sure to ask your doctor or nurse.
HH-I-12 7/80, Revised 3/08 Copyright 1980-2008, Nationwide Children's Hospital


