Hereditary Multiple Osteochondromas
Hereditary multiple osteochondromas is a genetic condition that causes benign bone tumors to grow.
What Is Hereditary Multiple Osteochondromas?
Hereditary multiple osteochondromas (HMO) is a rare genetic disorder in which persons develop non-cancerous (benign) bone tumors called osteochondromas. The condition is also known as multiple osteochondromas (MO), multiple hereditary exostosis (MHE) or hereditary multiple exostosis (HME).
A child is not born with these tumors. The tumors develop by ages 10-12, median age of 3. Tumors are commonly found during other procedures or X-rays, or a bump may be felt.
Hereditary means that one parent has a gene that is passed to a child. Even if the parent has the gene for HMO, the parent may not have the disease. The risk of passing the gene is 50%. In most cases (90%), people develop HMO when the gene is present. In very rare cases (10%), an unexplained genetic mutation can occur and cause HMO. Once children reach maturity and growth plates close, no new tumors develop. Most patients live healthy, active lives.
HMO is rare. It affects males more than females.
What Are the Signs and Symptoms of Hereditary Multiple Osteochondromas?
Osteochondromas form when cells grow abnormally on the flat surface of the cartilage end of bones. Cartilage is connective tissue that protects joints and bones and acts like a shock absorber. Knees, shoulders, ankles and wrists are the most common sites for osteochondromas. These bony tumors do not spread from one location to another. They are typically found on extremity long bones (bones longer than they are wide) or near growth plates. The spine, pelvis, scapula, ribs and other rare sites can be affected. Some individuals have a few benign tumors, and some have over 100.
Children often do not have symptoms. Tumors can be seen on X-rays. Sometimes they are found on a radiology test done for a different reason. This is called an incidental finding.
Children may develop a bump they can feel near a joint. Because these bumps don’t hurt, children often do not tell caregivers about them. As patients develop more lesions or they begin to have symptoms, they seek treatment. Osteochondromas also can cause pain if near a joint or cause an abnormal change in movement of a joint.
Pain can occur if the tumor affects soft tissue or other structures. Tumors can grow near nerves and compress them. This causes numbness in the area, which can affect joint movement as well.
How Is Hereditary Multiple Osteochondromas Diagnosed?
A thorough patient and family history and exam is the first step. If there is no known family history, and there are several tumors, a referral to a genetics physician will be made.
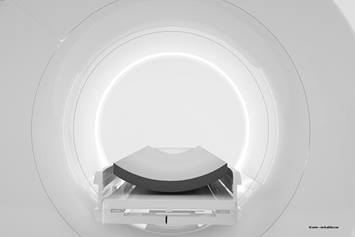
X-rays are typically the first and only radiology test needed. Patients often have X-rays done for other concerns and the bony lesion is seen. CT (computed tomography) and/or MRI (magnetic resonance imaging) may be necessary if the diagnosis needs confirmed, an initial screening is warranted, or there is a need to follow tumors over time.
A biopsy (a sample of the tissue of the affected bone) may be needed if the doctor thinks the tumor is cancerous (malignant) or if there is an unusual (atypical) appearance of the bone lesion. When one of the tumors is removed due to pain or other symptoms, pathology will confirm the diagnosis.
If a tumor develops when a child is younger, the tumor often grows larger. Limb length discrepancy (LLD) may develop if tumors affect growth in one limb. This may cause one limb to be shorter or one limb to be bowed. Some patients may be referred to the limb-lengthening clinic.
Short stature, joint dislocation, fracture, bone deformity, restricted joint movement or compression of peripheral nerves are some of complications that may require treatment and/or referral to other specialties. There is a rare chance of developing osteochondrosarcoma (cancer) in 1-5% of patients.
How Is Hereditary Multiple Osteochondromas Treated?
No medical treatment is currently available, but several research projects are being conducted. Osteochondromas will be removed if the doctor thinks they are malignant (which is very rare). They may be removed if they cause pain, altered function or neuromuscular-skeletal abnormality. Physical therapy can help with joint function and strengthening as needed or after surgery. Surgery is often outpatient and tolerated very well.
Your child will be seen on a regular basis until they have matured. Visits start at 3-6 month intervals then as they get older, 12 month visits are standard. Visits are scheduled prior to leaving a clinic appointment.