Pulmonary Hypertension
Pulmonary Hypertension is a term to describe a rare disease in which the blood pressure in the lungs is higher than normal.
About Pulmonary Hypertension
Pulmonary Hypertension is a term to describe a rare disease in which the blood pressure in the lungs (pulmonary artery system) is higher than normal. The staff of the Adolescent and Adult Congenital Heart Disease Program at Nationwide Children's Hospital is dedicated to providing advanced therapy for this condition.
Pulmonary Hypertension is a term to describe a rare disease in which the blood pressure in the lungs (pulmonary artery system) is higher than normal. The blood pressure that is measured on your arm by a cuff reflects systemic or your body’s blood pressure. Normal systemic blood pressure is 120/80 mmHg. Normal blood pressure within the lungs is much lower and much more difficult to evaluate. Normal blood pressure in the lungs is 15 -25 mmHg, or about 1/5th the bodies blood pressure.
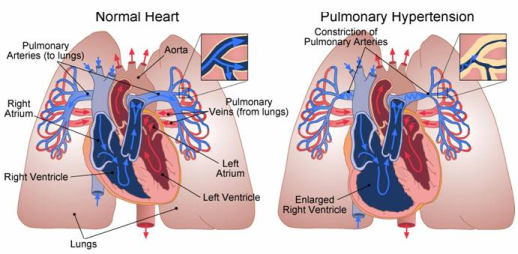
Pulmonary Hypertension results when the blood vessels constrict (tightens). Over time this constriction causes fibrosis (scars) of the vessel and higher pulmonary blood pressure. The chambers on the right side of the heart (right atrium and right ventricle) have difficulty pumping blood out to the pulmonary artery and through the lungs. The strain on the heart to overcome this high pressure and constriction causes the heart to become enlarged and weak. Eventually the heart cannot keep up with the body’s demands. This is known as heart failure.
Pulmonary Hypertension can be classified into two groups:
- Idiopathic or Primary Pulmonary Hypertension - Pulmonary Arterial Hypertension (PAH) that is not the result of another medical condition. This means that your doctor may not be able to explain to you why you or your child may have developed pulmonary hypertension. Although idiopathic pulmonary hypertension affects men, women and children it is most common in women between the ages of 20-45 years of age. It is possible that there is a family or hereditary link associated with the disease. It is also believed that the use of certain drugs such as diet pills (Redux, Fen-phen), street drugs like cocaine or amphetamines and disease such as AIDS and liver disease may trigger the disease.
- Secondary Pulmonary Hypertension - Pulmonary Hypertension that is associated with or the result of another medical condition.
Signs and Symptoms of Pulmonary Hypertension
The signs and symptoms of Pulmonary Hypertension include:
- Fatigue
- Shortness of Breath
- Chest Pain
- Dizziness
- Fainting (syncope)
- Swollen ankles and legs (edema)
- Swelling in abdomen (ascities)
- Rapid pulse or palpitations of the heart
Conditions that Cause Pulmonary Hypertenstion
There are many diseases that can cause pulmonary hypertension (PH). The following is a brief explanation of each of these conditions.
PH Associated with Connective Tissue Diseases
Connective Tissue Diseases such as scleroderma, CREST syndrome, rheumatoid arthritis, and systemic lupus are autoimmune disease associated with pulmonary hypertension. Of these conditions scleroderma is the most common disease link to pulmonary hypertension.
PH Associated with Hypoxemia (Low Oxygen)
Oxygen opens the lung passages. When the body is deprived of oxygen it can cause constriction of the lung vessels resulting in pulmonary hypertension. Diseases that affect lung breathing passages and decrease oxygen include asthma, emphysema, chronic bronchitis, interstitial lung disease and cystic fibrosis.
Another form of lung disease related to low oxygen and periods of not breathing (apnea) during the sleep cycle – is called sleep apnea. Obstructive Sleep Apnea (the inability to breath due to blocked airway passage) is the most common form found in overweight middle aged adults. Treatment with breathing machines (CPAP/Bi Pap) during sleep helps improve oxygen levels.
PH Associated with Congenital Heart Disease
A child may be born with a hole in the septum of the heart. The septum is the wall that separates the right and left side of the heart.
If the hole is between the two upper chambers, it is called atrial septal defect (ASD). Most ASD’s are repaired during childhood; however, it is possible to repair these holes at any age if there is little to no signs of pulmonary hypertension that exists.
If the hole is between the two lower chambers it is called a ventricular septal defect. (VSD). Ventricular septal defects are the most common congenital heart defects. When a defect is present, blood can flow across the hole from the left side of the heart to the right. Children born with VSD’s are more likely to develop pulmonary hypertension than those with ASD’s if they are not closed early in life. The reason is because there is excessive blood flow and pressure through the hole into the right side of the heart and lungs that results in enlargement of both the right atrium and ventricle. Over time the extra blood flow into the lungs causes damage to the blood vessels resulting in pulmonary hypertension.
PH Associated with Left Ventricular Diastolic Dysfunction
The heart cycle is divided into two phases, systole and diastole. Systole is when the heart is pumping blood out to the lungs and body. After the ventricles eject the blood they must relax and refill with blood to prepare again for pumping. This relaxation phase is known as diastole. The ventricles can become stiff over time not allowing the ventricles to fill completely with blood during diastole. The stiffness of the ventricles and inability to relax causes the pressure to rise on the left side of the heart, and eventually the pressure in the lungs rises. This condition is known as diastolic dysfunction. Diastolic dysfunction may occur with normal aging but is also associated with chronic high blood pressure, coronary artery disease (blockage of the coronary arteries) and many forms of cardiomyopathies (failure of the heart muscle).
Diastolic dysfunction can only be diagnosed by heart catheterization. The data that the doctor obtains during the heart catheterization will help identify this type of heart disease. Although diastolic dysfunction is a form of pulmonary hypertension the treatment is different and the goal is to relax the left ventricle using specific drugs such as nitrates. It is also important to control the body’s (systemic) blood pressure, treat coronary artery disease and control lung congestion with diuretics.
PH Associated with Chronic Thromboembolic/Embolic Disease
A thrombus or thromboembolism is a blood clot that blocks the passage of blood through a vessel. If blood clots travel to the lung, the obstruction may lead to pulmonary hypertension. Sometimes blood clots in the lungs do not cause symptoms. Pulmonary Hypertension caused by blood clots is rare and may require surgical removal of the clots by a procedure called thromboendarterectomy.
There are many diseases that can cause pulmonary hypertension (PH). The following is a brief explanation of each of these conditions.
How is Pulmonary Hypertension Diagnosed?
Testing for pulmonary hypertension includes:
-
A complete history and physical exam.
-
An electrocardiogram (ECG) may show a strain on the right side of your heart
-
Blood Tests to evaluate if you have any form of collagen vascular disease
-
A chest CT Angiogram to assess for lung disease and detect blood clots in the lung circulation
-
A pulmonary function test to measure lung capacity ( how much air the lungs inhale and exhale). Poor lung capacity reflects the degree of damage or deterioration of the lungs.
-
An exercise test called a six minute walk. You will be required to walk on a flat surface as fast as you can for six minutes to evaluate how much exercise you can do before you have symptoms.
-
An echocardiogram and cardiac catheterization
The echocardiogram can demonstrate the pump function of the heart and the quality of blood flow through the heart valves. Although this is a good test it is not the most accurate or reliable test for the diagnosis of pulmonary hypertension.
The only precise way to diagnose pulmonary hypertension is with a cardiac catheterization. A cardiac catheterization reveals important information including:
-
How well the heart is working (known as cardiac output)
-
How high the pressures are within the pulmonary artery (mean pulmonary artery pressure)
-
How stiff or tight the pulmonary blood vessels are (known as pulmonary vascular resistance)
-
How well medicines are working
Patients living with Pulmonary Hypertension have several treatment options to improve their quality of life.
Treatment Options
Nationwide Children's Hospital is dedicated to providing advanced therapy for pulmonary hypertension. Patients living with pulmonary hypertension have several treatment options to improve symptoms of the disease and their quality of life, available therapies include:
-
Intravenous Flolan
-
Intravenous Remodulin
-
Subcutaneous Remodulin
-
Endothelin Antagonists: Tracleer (Bosentan)/Sitaxsentan (Thelin)/Ambrisentan
-
Phosphodiesterase type 5 inhibitor: Viagra (Sildenafil)
-
Inhaled Iloprost (Ventavis)
-
Clinical Research of new medications
Preparing for Your Heart Catheterization
Before the heart catheterization a doctor will explain the risks and benefits of this procedure. You will remain without food or drink 12 hours before the procedure. You may take you regular a.m. medications on the day of the procedure however you should hold any blood thinners or diabetic medications.
Possible Risks Associated with a Heart Catheterization
-
Bleeding at the catheter insertion site
-
Arrhythmia (abnormal heartbeat)
-
Allergic reaction to the dye
The Procedure
You will be given medication to help you relax however you will remain awake during the procedure. The area where the catheters will be inserted will be numbed with a local anesthetic. The catheterization is performed by placing a flexible plastic tube into a large vein in the groin area known as the inferior vena cava.
This catheter is manually moved forward by the doctor toward your heart. The doctor uses x-ray pictures to help guide the catheter. Once the catheter is inside your heart, blood pressure is obtained in the right atrium, right ventricle and pulmonary artery. With this data the doctor then calculates the strength of your heart and the stiffness or resistance of the pulmonary vessels. This is known as a right heart catheterization.
Normal Blood Pressures
-
Right Atrium 0-8 mmHg
-
Right Ventricle 15-30 mmHg
-
Pulmonary Artery Mean 15-25mmHg
The diagnosis of pulmonary hypertension is elevation of the mean pulmonary artery pressure greater than 25 mmHg. Elevation of mean pulmonary artery pressure can range from mild to severe.
-
Mild: 26-35 mmHg
-
Moderate: 36-45mmHg
-
Severe: above 45 mmHg
It is common for patients to focus on their pulmonary pressure. However, it is the strength of the heart (cardiac output) and tightness of the pulmonary vessels (pulmonary vascular resistance) that corresponds with symptoms and severity of the disease.
-
Normal Cardiac Output = 4-8 L/min
-
Normal Pulmonary Vascular Resistance = less than 3 units
After the Procedure
You will have a small puncture wound in your groin and be required to lay flat for 2-6 hours following your heart catheterization to recover. You may return to work and full activity 24-48 hours. You may resume your blood thinners after your heart catheterization.