Sickle Cell Disease (SCD) and Acute Chest Syndrome (ACS)

Sickle cell disease (SCD) is an inherited (passed down from parents) blood disorder. It affects a part of the red blood cell called hemoglobin. Hemoglobin carries oxygen to different parts of the body.
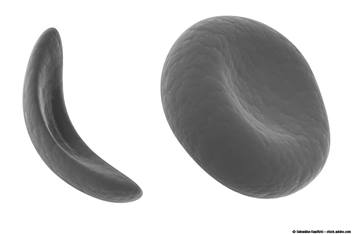
A person with SCD makes a different kind of hemoglobin, called sickle hemoglobin. Instead of being round and smooth like normal red blood cells, blood cells with sickle hemoglobin are shaped like a banana. The sickle shape causes the red blood cells to stick together and clog small blood vessels. When this happens, parts of the body cannot get enough oxygen. Not having enough oxygen can cause pain and may damage the body.
Acute Chest Syndrome
Acute chest syndrome (ACS) is a group of symptoms that occurs when sickled cells clump together in the lungs (Picture 1).
ACS can be triggered by:
- a lung infection, like pneumonia (new.MOAN.yuh)
- an episode of pain - before, during or after the episode, even when a child is in the hospital
- surgery and anesthesia
ACS can be life-threatening if not treated right away.
Symptoms of ACS
- chest pain
- fever at or higher than 101° F (Fahrenheit) or 38° C (Celsius)
- tightness in chest
- breathing very fast
- cough
- shortness of breath
Diagnosis and Treatment
- To diagnose ACS, the health care provider will order blood tests and a chest X-ray.
- To treat ACS, most children are admitted to the hospital and watched very closely. Your child will get:
- antibiotics to treat a possible lung infection, like pneumonia
- medicines to help with breathing
- oxygen, if their blood oxygen level is low
- a blood transfusion, if needed
Prevention
The main way to prevent ACS is to get air down deep into the small airways of the lungs. Taking deep breaths will keep them open. When the small airways are clogged, sickled cells are more likely to clump together and cause ACS.
Here are some things your child can do in the hospital and at home to breathe more deeply:
- Get out of bed and walk at least 2 or 3 times a day while in the hospital. At home, keep active. People tend to breathe less deeply when lying down or not moving.
- Breathe deeply, even when in pain. When in pain, it is easy to hold your breath or pant without realizing it.
- Use an incentive spirometer (Picture 2) in the hospital and when you go home. This device will help your child take slow deep breaths and fill the lungs with air. Using an incentive spirometer is the BEST way to prevent ACS.
How to Use the Incentive Spirometer
Tell your child to:
- Sit up straight on the edge of the bed with feet on the floor. If they cannot sit on the edge of the bed, they need to sit up in bed as far as they can.
- Hold the incentive spirometer in an upright position.
- Breathe out normally.
- Place the mouthpiece in their mouth and seal their lips tightly around it (Picture 3).
- Breathe IN slowly and as deeply as possible to raise the blue piston toward the top of the column. The blue coach indicator should be inside the blue outlined area (see Picture 3, page 2).
- Hold their breath as long as possible (for 3 to 5 seconds) and then slowly breathe out. Let the piston fall to the bottom of the column.
- Rest for a few seconds and breathe normally.
- Repeat steps 3 through 7 at least 10 times every 2 hours while awake, or as ordered by your child’s health care provider.
- Set the blue indicator to the highest point where they were able to raise the piston to in the past. Use the indicator as a goal to work toward or to go even higher. The nurse or respiratory therapist may help set this goal.
- After each set of 10 deep breaths, practice coughing. This will bring up mucus and help clear the lungs. If they have an incision, support the incision when coughing by placing a pillow firmly against it.
Note: Breathing deeply might hurt. It is important to do it anyway to prevent ACS or a lung infection.
While in the hospital, if breathing deeply causes intense pain, your child can get pain medicine 20 minutes before using the incentive spirometer (or push the button on the pain medicine pump if one is being used).
Your health care provider will give instructions on how often to use the incentive spirometer at home after discharge from the hospital.
When to Call 911
Call for emergency help (911) if your child has any of these signs:
- unresponsive
- unable to wake up
- trouble breathing
- cannot move a body part
- cannot move a body part
Follow-up
Your child will have appointments at the Sickle Cell Clinic at Nationwide Children’s Hospital. If your child is ill or if you have any questions, call:
- During the day, the Sickle Cell Clinic (614) 722-8914
- On evenings and weekends, (614) 722-2000 and ask for the hematologist on call.
- Monday through Friday between 8 a.m. to 4:30 p.m., the Sickle Cell Nurse (614) 722-891 for non-urgent calls.
Sickle Cell Disease and Acute Chest Syndrome (PDF)
HH-I-225 © 2003, Revised 2021, Nationwide Children’s Hospital